摘要
人類陰道被多樣化的微生物群所定殖,這些微生物構成了正常的細菌群和真菌群。乳酸桿菌是從健康人類陰道中最常分離出的微生物,包括卷曲乳酸桿菌 [Lactobacillus crispatus]、加氏乳桿菌 [Lactobacillus gasseri]、陰道乳桿菌 [Lactobacillus iners] 和詹氏乳桿菌 [Lactobacillus jensenii]。這些陰道乳酸桿菌被認為能通過控制病原菌的數量來防止其入侵。然而,陰道生態系統的破壞會導致病原菌過度生長,從而引發複雜的陰道感染,如細菌性陰道病(BV)、性傳播感染(STIs)和外陰陰道念珠菌病(VVC)。諸如月經、懷孕、性行為、抗生素無節制使用和陰道沖洗等誘發因素可能改變微生物群落。因此,陰道微生物群的組成在決定陰道健康中扮演重要角色。由於乳酸桿菌被普遍認為是安全的(GRAS),它們被廣泛用作對抗陰道病原菌的傳統抗菌治療之外的替代方案之一,用於預防慢性陰道炎和恢復陰道生態系統。此外,乳酸桿菌作為預防措施的長期給藥效果也已被充分證實。本篇綜述旨在強調乳酸桿菌衍生物(即表面活性分子)在開發陰道感染療法中的有益效果,包括抗生物膜、抗氧化、抑制病原菌和免疫調節活性。我們還討論了在推廣人類健康中使用乳酸桿菌衍生物的當前挑戰。在本篇綜述中,我們希望為開發乳酸桿菌衍生物作為陰道健康中傳統益生菌療法的補充或替代醫學提供見解。
關鍵詞: 陰道微生物群、陰道生態系統、益生菌、乳酸桿菌、乳酸桿菌衍生物、表面活性分子
背景
人類微生物群計畫(HMP)和整合HMP(iHMP)由美國國立衛生研究院(NIH)資助。它們是跨學科努力,致力於對腸道、陰道、口腔和皮膚群落的微生物群進行分析 [1, 2]。這兩個計畫旨在揭示這些解剖部位的微生物特性、分佈和宏基因組學 [3]。HMP的發現被認為對於建立微生物群變化與疾病發病機制的關係以及識別診斷用的生物標誌物具有重要意義 [4]。
人類陰道微生物群包含多樣化的有益微生物和機會性病原菌,這些微生物棲息於陰道環境中 [5, 6]。為了理解人類陰道內的微生物群,已開發出多種涉及“-omics”技術的方法。研究微生物群落的常用分子方法包括聚合酶鏈反應-變性梯度凝膠電泳(PCR-DGGE)、DNA焦磷酸測序、螢光原位雜交(FISH)、定量PCR和微陣列 [7]。此外,其他現代“-omics”技術,如代謝組學、宏基因組學、宏轉錄組學和蛋白質組學,已開始重新激發對微生物群落功能活動發現的研究 [8]。現代多組學數據的整合能夠通過微生物和代謝輪廓與其在調節人類健康中的作用的關聯,解碼複雜微生物群落的功能見解 [8]。迄今為止,大多數人類微生物群研究利用16S rRNA基因測序來識別複雜微生物群落,因其在推斷導致疾病的某些微生物群落的代表性方面具有可行性 [9]。自從評估人類微生物多樣性的技術進步以來,Ravel等人 [10] 已成功利用先進的高通量測序技術識別出五種不同的細菌群落。人們認為陰道環境中的原生微生物群與宿主處於共生關係 [11]。真菌,尤其是念珠菌屬,很可能作為共生菌存在於陰道黏液層中,並與其他細菌一起構成複雜的陰道生態系統 [12, 13]。研究表明,生育年齡女性的微生物群和真菌群組成的波動導致了陰道群落的時間動態 [11]。事實上,這種波動受到荷爾蒙變化、年齡、性行為和抗菌藥物使用的影響 [14–17]。陰道中的微生物失調導致機會性病原菌過度生長,最終促成疾病的發病 [18]。
陰道菌群失調反映了陰道微生物群落的破壞,並經常與多種婦科疾病相關。多項研究顯示,陰道菌群失調與陰道感染增加有關,如細菌性陰道病(BV)、外陰陰道念珠菌病(VVC)、性傳播感染(STIs),即滴蟲病、人類乳突病毒(HPV)感染、沙眼衣原體(CT)感染、人類免疫缺陷病毒(HIV)易感性和生殖器皰疹感染 [19–23]。陰道菌群失調的一個顯著特徵是陰道pH值的變化。最近一項研究報告,與健康女性相比,BV、CT和VVC患者的陰道pH值顯著升高,這是由於乳酸濃度降低引起的 [24]。陰道微生物群落的轉變若不加以處理,還可能導致嚴重的婦科問題,如流產、早產和低受孕率 [25]。總體而言,維持陰道微生物群的和諧平衡對於促進健康的陰道生態系統至關重要。
人類微生物群知識的進展加速了使用有益微生物進行活體生物治療的新探索步伐 [26]。此前,通過糞便菌群移植(FMT)的活體生物治療已被證明在治療復發性難辨梭菌感染中成功 [27]。由於FMT的成功,類似的方法使用陰道微生物群移植(VMT)可能有效治療棘手的陰道感染。最近,第一例VMT被報導能夠在復發性BV患者中重建以乳酸桿菌為主的微生物群,且未觀察到不良反應 [28]。此外,接受乳酸桿菌與抗生素聯合給藥的患者也顯示出對復發性BV的傾向降低 [29]。在一項類似研究中,使用甲硝唑與鼠李糖乳桿菌 [L. rhamnosus] GR-1 和羅伊氏乳桿菌 [L. reuteri] RC-14 的聯合療法成功治療了88%的BV患者,而僅接受甲硝唑治療的患者恢復率為40% [30]。研究表明,這些有益效果部分與細胞表面活性分子(SAMs)相關,如肽聚醣(PG)、脂磷壁酸(LTA)、生物表面活性劑(BS)和胞外多醣(EPS) [31, 32]。事實上,乳酸桿菌SAMs已被證明能拮抗多種細菌和真菌病原菌,如白色念珠菌 [Candida albicans]、金黃色葡萄球菌 [Staphylococcus aureus]、變形鏈球菌 [Streptococcus mutans]、大腸桿菌 [Escherichia coli]、綠膿桿菌 [Pseudomonas aeruginosa] 和沙門氏菌 [Salmonella typhimurium] [33–35]。因此,進一步了解乳酸桿菌及其衍生物(即SAMs)可能為開發由陰道菌群失調引起的感染的新療法鋪平道路。
在過去十年中,對陰道微生物群的調查呈指數級增長。這些研究揭示了塑造女性陰道微生物群獨特組成的微生物群落多樣性 [10, 24, 36–38]。這些研究的共同發現表明,以乳酸桿菌為主的群落在健康狀態的陰道中可能被觀察到,而在疾病狀態的陰道中報告了較高的陰道pH值(較不酸性)。此外,一些女性的陰道微生物組成高度動態,這是由於多個誘發宿主因素最終影響宿主-微生物相互作用。截至目前,若存在單一根本原因,陰道菌群失調的確切原因仍有待確定。在本篇綜述中,我們旨在提供女性原生陰道微生物群和真菌群的概覽。此外,我們致力於強調乳酸桿菌及其衍生物(即SAMs)在控制陰道病原菌以促進陰道健康中的潛在作用。
女性原生陰道微生物群
健康的人類陰道以乳酸桿菌為主,已報導真菌分類的邊緣存在 [39]。通常,有益細菌群落與人類宿主以互利共生方式共存,通過保護宿主陰道環境免受病原微生物的定殖,而宿主為細菌生長提供營養 [11]。乳酸桿菌的定殖和主導地位是健康陰道微生物群的重要特徵,通常由卷曲乳酸桿菌 [Lactobacillus crispatus]、加氏乳桿菌 [Lactobacillus gasseri]、陰道乳桿菌 [Lactobacillus iners] 和詹氏乳桿菌 [Lactobacillus jensenii] 等物種組成 [10, 40, 41]。人類陰道微生物群的組成變化可能在不同生命階段發生,包括嬰兒期、青春期、懷孕和更年期階段 [42]。事實上,荷爾蒙變化、抗生素無節制使用、月經和陰道沖洗是引導人類陰道微生物群時間變化的常見因素 [6, 43, 44]。
健康陰道中主要乳酸菌(LAB)的相對豐度決定了細菌群落類型,稱為群落狀態類型(CSTs) [10]。CSTs 分為 CST I、II、III、IV、V,分別由卷曲乳酸桿菌 [L. crispatus]、加氏乳桿菌 [L. gasseri]、陰道乳桿菌 [L. iners]、包括乳酸桿菌和細菌性陰道病相關細菌(BVAB)的多微生物群以及詹氏乳桿菌 [L. jensenii] 主導(圖1) [6, 10]。雖然 CST I、III 和 IV 已得到廣泛研究並在女性中常見,但 CST II 和 V 在女性中卻很少見 [45, 46]。事實上,DiGiulo 等人 [47] 和 van de Wijgert 等人 [46] 在其研究中報告,健康女性的陰道微生物群部分屬於 CST II 和 V。Gajer 等人 [6] 進一步將 CST IV(缺乏特定乳酸桿菌物種的顯著豐度)細分為 CST IV-A 和 CST IV-B [6]。根據 Gajer 等人,CST IV-A 通常含有適量的陰道乳桿菌 [L. iners] 以及厭氧菌,如棒狀桿菌 [Corynebacterium]、細金菌 [Finegoldia]、鏈球菌 [Streptococcus] 或厭氧球菌 [Anaerococcus],而 CST IV-B 則具有顯著更高數量的 BVAB [6]。
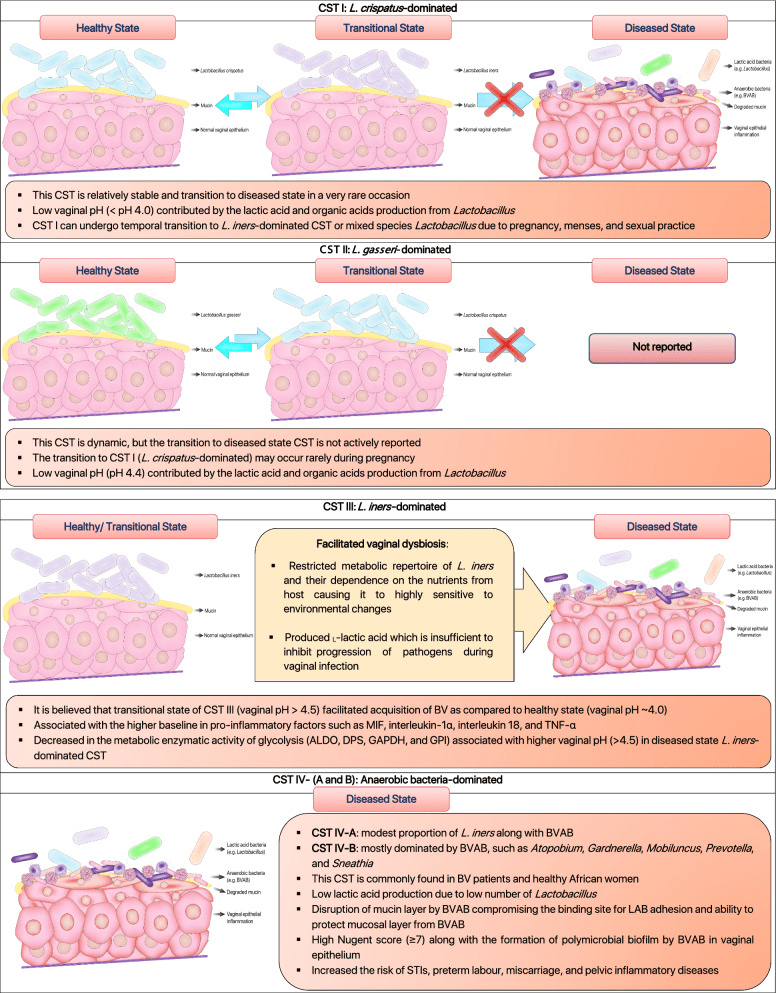

根據科學文獻對人類陰道群落狀態類型(CSTs)的示意說明。陰道微生物群的健康與疾病狀態可根據其各自特性分為五種常見的CSTs。這些CSTs主要由卷曲乳酸桿菌 [L. crispatus]、加氏乳桿菌 [L. gasseri]、陰道乳桿菌 [L. iners]、細菌性陰道病相關細菌(BVAB)和詹氏乳桿菌 [L. jensenii] 主導 [6, 10, 47, 96, 262, 263]。
陰道中乳酸桿菌的存在協調了一種獨特的炎症模式,促成了不同的群落狀態類型(CSTs)。值得注意的是,CST III 和 CST IV 中陰道乳桿菌 [L. iners] 的存在與較高的促炎因子基線水平相關,如巨噬細胞遷移抑制因子(MIF)、白細胞介素-1α、白細胞介素-18 和腫瘤壞死因子-α(TNF-α),這些因子負責激活陰道中的炎症反應 [48]。以卷曲乳酸桿菌 [Lactobacillus crispatus] 主導的陰道微生物群(CST I)總是與健康的陰道相關,而以陰道乳桿菌 [L. iners] 主導的陰道環境(CST III)更容易發生陰道菌群失調(圖1) [49, 50]。多項研究表明,卷曲乳酸桿菌 [L. crispatus] 對性傳播感染(STIs)、細菌性陰道病(BV)和外陰陰道念珠菌病(VVC)的保護作用,與其產生乳酸和細菌素以維持陰道健康狀態的能力密切相關 [51, 52]。與此同時,陰道乳桿菌 [L. iners] 缺乏必需氨基酸合成能力,迫使其嚴重依賴宿主提供的外部氨基酸 [53]。其有限的代謝能力和對宿主營養的依賴使其對環境變化高度敏感 [53]。此外,它還產生了一種獨特的乳酸異構形式(L-乳酸),這種形式不足以在陰道感染期間抑制病原菌的進展 [54, 55]。另外,大量研究顯示,人類陰道微生物群的組成因個體而異,並受到荷爾蒙(如懷孕和月經)以及種族的顯著影響 [10, 56]。荷爾蒙尤其是雌二醇的影響,事實上,可以刺激CST I(以卷曲乳酸桿菌 [L. crispatus] 主導)向CST III(以陰道乳桿菌 [L. iners] 主導)或混合乳酸桿菌群落的轉變,但很少轉向疾病狀態的陰道群落(圖1) [6, 46]。此外,疾病狀態(CST IV)和促進BV狀態(CST III)的陰道群落在撒哈拉以南非洲地區更為常見 [6, 10]。可以設想,這些群體的遺傳因素可能改變陰道免疫反應,從而有利於陰道乳桿菌 [L. iners] 和引起陰道菌群失調的病原共生菌的定殖 [56, 57]。正如已指出的,陰道微生物群落的特性研究極大地擴展了我們對健康與異常陰道微生物群之間關係的知識。在陰道乳桿菌 [L. iners] 基因組中發現的前噬菌體表明,噬菌體可能影響乳酸桿菌在陰道生態系統中的適應策略和豐度 [58]。因此,未來需要進一步研究以闡明乳酸桿菌噬菌體的存在及其對健康與疾病狀態陰道的貢獻。
大多數亞洲和白人女性的核心陰道微生物群分別由80.2%和89.7%的乳酸桿菌主導 [10]。相比之下,乳酸桿菌並非黑人和西班牙裔女性陰道微生物群中唯一的優勢屬(分別僅占59.6%和61.9%) [10]。一項針對151名女性(65名HPV陽性,86名HPV陰性)的橫斷面研究顯示,HPV與厭氧菌(如多形擬桿菌 [Bacteroides plebeius]、盧氏無枝酸桿菌 [Acinetobacter lwoffii] 和口腔普雷沃氏菌 [Prevotella buccae])的高豐度顯著相關 [59]。這一發現表明,陰道微生物群的多樣性增加顯著提高了HPV感染的風險 [59]。可以設想,陰道微生物群的破壞可能影響宿主對HPV感染的先天免疫,從而導致宮頸癌的發展 [60]。此外,Lee 等人 [61] 還揭示,陰道菌群失調與HPV感染密切相關。HPV感染女性的陰道微生物群中普雷沃氏菌 [Prevotella]、血鏈球菌屬 [Sneathia]、雙桿菌屬 [Dialister] 和桿菌屬 [Bacillus] 的豐度較高,而乳酸桿菌的豐度低於健康女性 [61]。此外,以乳酸桿菌低豐度和陰道加德納菌 [G. vaginalis] 主導為特徵的陰道微生物群失調,與HPV感染和宮頸腫瘤發展顯著相關 [62]。另外,乳酸桿菌低豐度以及陰道中加德納菌 [Gardnerella]、布魯氏菌 [Brucella]、血鏈球菌屬 [Sneathia] 和其他雜菌的高比例,在HPV和生殖器疣感染患者中較為常見 [63]。總之,陰道微生物群失衡與HPV相關感染的風險密切相關。簡言之,針對陰道菌群失調的干預治療可能降低HPV感染和宮頸癌發展的風險 [64]。
與陰道微生物群分析相比,人類陰道真菌群仍未被充分研究。首次針對陰道真菌群的高通量測序由Drell及其同事於2013年進行 [39]。根據Drell 等人 [39] 的研究,從健康的愛沙尼亞女性中獲得了196個真菌操作分類單元(OTUs);最優勢的門是子囊菌門(Ascomycota,58.0%),其次是未指定的真菌OTUs(39.0%)和擔子菌門(Basidiomycota,3.0%)。子囊菌門中最常見的OTUs(糖酵母目,Saccharomycetales)是念珠菌屬(Candida,37.0%),主要包括白色念珠菌 [C. albicans](34.1%)、克魯斯念珠菌 [Candida krusei](2.3%)、營養念珠菌 [Candida alimentaria](在該研究中報導為 Candida sp. VI04616,0.3%)、近平滑念珠菌 [Candida parapsilosis](0.3%)和都柏林念珠菌 [Candida dubliniensis](0.04%) [39]。類似地,少數研究也顯示,念珠菌群落在無症狀和健康女性中存在 [65, 66]。此外,Ward 等人 [67] 報告,無論分娩方式如何,嬰兒的優勢真菌群與母親陰道的真菌種類相同(白色念珠菌 [C. albicans]) [67]。此外,嬰兒中白色念珠菌 [C. albicans] 的定殖在通過母親垂直傳播後顯而易見 [68]。總之,這些發現表明,白色念珠菌 [C. albicans] 可以在不引起任何症狀性感染的情況下定殖陰道。與此同時,越來越多的研究還強調了一些風險因素,如荷爾蒙、糖尿病、口交、陰道內沖洗、自行使用抗真菌藥和抗生素、宮內節育器的使用以及會陰撕裂,這些因素與VVC的發生顯著相關 [69–71]。關於陰道相關感染的人類微生物群分析的選定出版物總結於表1。
表1.
全球人類陰道微生物群研究(2007-2020年)及其主要發現
| 國家/地區 | 研究設計 | 主要發現 | 參考文獻 |
|---|---|---|---|
| 比利時蒂嫩 | 26名女性:11名健康、5名BV、7名VVC、3名BV-VVC<br>年齡:23-40<br>橫斷面研究<br>使用PCR-變性梯度凝膠電泳(PCR-DGGE)和16S rRNA實時PCR分析進行微生物分析 | PCR-DGGE顯示健康女性的陰道微生物群隨時間穩定,以嗜酸乳桿菌 [L. acidophilus]、加氏乳桿菌 [L. gasseri]、陰道乳桿菌 [L. iners] 和陰道乳酸桿菌 [L. vaginalis] 為主導;少量陰道加德納菌 [G. vaginalis] 與乳酸桿菌共存於一些健康女性中,可能作為哨兵物種,對環境、生物和物理變化敏感;BV患者報告乳酸桿菌豐度低,同時BV相關細菌(如陰道加德納菌 [G. vaginalis]、陰道阿托波菌 [A. vaginae]、鉤端螺旋體 [Leptotrichia]、大球菌 [Megasphaera]、普雷沃氏菌 [Prevotella]、葡萄球菌 [Staphylococcus]、鏈球菌 [Streptococcus]、韋榮氏菌 [Veillonella])增加;VVC患者中非H2O2產生的陰道乳桿菌 [L. iners] 增加,嗜酸乳桿菌 [L. acidophilus]、加氏乳桿菌 [L. gasseri] 和陰道乳酸桿菌 [L. vaginalis] 豐度減少 | [264] |
| 美國愛荷華州 | 橫斷面研究<br>42名女性:21名健康、21名RVVC感染(2年內≥4次)<br>年齡:18-40<br>使用16S rRNA末端限制片段多態性(T-RFLP)進行微生物分析 | VVC感染女性與健康女性在細菌群落和陰道pH值上無顯著差異;大多數RVVC患者無症狀;未發現陰道群落與RVVC風險之間的相關性 | [265] |
| 美國喬治亞州和馬里蘭州 | 橫斷面研究<br>396名非孕婦<br>年齡:12-45<br>使用條碼16S rRNA測序進行微生物分析 | 引入五種陰道CSTs(I、II、III、IV、V)以根據乳酸桿菌豐度分析陰道微生物群狀態;黑人和西班牙裔女性的陰道pH值較高(pH 4.7-5.5),相較於亞洲和白人女性(pH 4.2-4.4);CST III(以陰道乳桿菌 [L. iners] 主導)和CST IV(以BVAB主導)在黑人和西班牙裔女性中更常見 | [10] |
| 中國 | 95名非孕婦:30名健康、39名VVC、16名BV-VVC、10名BV<br>橫斷面研究<br>使用條碼16S rRNA測序進行微生物分析 | 健康中國女性的陰道微生物群以乳酸桿菌為主,陰道pH值呈酸性(< pH 4.5);BV感染女性顯示陰道微生物群多樣性最高(乳酸桿菌豐度低);BV-VVC女性具有獨特模式,乳酸桿菌豐度較高;VVC單獨感染女性報告多樣的陰道微生物群,並在唑類治療後顯示如鏈球菌 [Streptococcus] 和陰道加德納菌 [Gardnerella] 主導的異常微生物群;BV-VVC女性在抗菌治療後乳酸桿菌豐度增加 | [266] |
| 愛沙尼亞 | 494名健康且無症狀的白人女性<br>年齡:15-44<br>橫斷面研究<br>使用條碼16S rRNA進行細菌分析,ITS測序進行真菌分析 | 健康且無症狀女性的陰道微生物群以乳酸桿菌為主;一些女性中也報導有BVAB(如陰道阿托波菌 [A. vaginae] 和陰道加德納菌 [G. vaginalis]),可分類為無症狀BV感染女性;陰道微生物群多樣性隨著陰道pH值升高而增加,且伴隨異味分泌物;念珠菌屬,尤其是白色念珠菌 [Candida albicans],仍是從無症狀女性中最常分離出的酵母菌 | [39] |
| 美國西雅圖 | 45名女性參與縱向研究(2007-2010)<br>治療:7、14、21、28天的甲硝唑治療<br>使用16S rRNA qPCR和數學建模進行細菌動態分析 | 治療第一天BVAB快速減少,過渡真空期內陰道乳桿菌 [L. iners] 豐度逐漸增加;治療對陰道加德納菌 [G. vaginalis] 無效,患者中BV復發頻繁 | [267] |
| 加拿大多倫多 | 182名孕婦(孕11-16週)<br>與先前非孕加拿大女性研究(n=310)比較微生物輪廓<br>使用通用引物cpn60測序進行微生物分析 | 以乳酸桿菌為主的CST孕婦相較於非孕婦具有較高乳酸桿菌豐度;孕婦報告較低的豐富度和多樣性(軟壁菌 [Mollicutes] 和脲原體 [Ureaplasma] 豐度低),與早產和流產風險低相關;荷爾蒙誘導的糖原生成可能為陰道細菌生長提供有利環境,解釋了孕婦比非孕婦攜帶更高細菌負荷 | [268] |
| 肯尼亞、南非、盧旺達(三地) | 80名女性參與陰道生物標誌物研究:40名健康、40名BV<br>8週縱向研究(連續五次訪問)<br>革蘭氏染色、qPCR、宮頸陰道沖洗液中可溶性免疫介質定量 | 79%的卷曲乳酸桿菌 [Lactobacillus crispatus] 主導微生物群女性伴隨陰道乳酸桿菌 [Lactobacillus vaginalis],而詹氏乳桿菌 [L. jensenii] 和加氏乳桿菌 [L. gasseri] 未出現;健康女性(正常Nugent評分)以陰道乳桿菌 [L. iners] 主導微生物群,因性活動和閉經與微生物群多樣性和陰道炎症顯著相關;BV感染女性(Nugent 7-10)報告乳酸桿菌低豐度,陰道加德納菌 [G. vaginalis]、陰道阿托波菌 [A. vaginae] 和雙歧普雷沃氏菌 [P. bivia] 豐度高,伴隨促炎細胞因子(IL-1β、IL-12)增加和抗蛋白酶elafin(IP-10)減少 | [269] |
| 美國馬里蘭大學 | 40名非孕婦<br>橫斷面研究<br>使用16S rRNA測序進行微生物分析<br>陰道溶血素(細胞毒性蛋白)定量 | CST-IV中陰道溶血素濃度高於CST-I微生物群高豐度女性;陰道乳桿菌 [L. iners] 主導微生物群(CST-III)女性報告中等濃度的陰道溶血素;乳酸桿菌缺乏的陰道微生物群中陰道加德納菌 [G. vaginalis] 豐度高,與陰道pH值、Nugent評分和陰道溶血素濃度增加相關 | [270] |
| 土耳其伊斯坦堡 | 28名健康白人女性:14名組織學子宮內膜異位症、14名健康<br>前瞻性觀察性隊列研究<br>使用16S rRNA宏基因組測序進行微生物分析 | 乳酸桿菌在健康和子宮內膜異位症診斷女性中仍是優勢屬;子宮內膜異位症診斷女性的陰道加德納菌 [G. vaginalis] 豐度顯著高於健康女性;子宮內膜異位症女性報告陰道和宮頸中無陰道阿托波菌 [A. vaginae],宮頸中大腸桿菌 [E. coli]、志賀氏菌 [Shigella]、鏈球菌 [Streptococcus] 和脲原體 [Ureaplasma] 豐度增加 | [271] |
| 美國馬里蘭大學公共衛生學院健康行為研究中心 | 39名女性:26名HPV陽性(14名高風險HPV)、13名HPV陰性<br>橫斷面研究<br>使用16S rRNA測序進行微生物分析,液相色譜質譜法進行陰道代謝物分析 | HPV陽性女性報告較高的生物胺(如腐胺和乙醇胺)濃度和較低的穀胱甘肽(GSH)、糖原和磷脂濃度,與HPV陰性女性相比;HPV陽性女性(CST-III陰道微生物群)也報告較高的生物胺和糖原相關代謝物濃度;HPV陽性女性(CST-IV陰道微生物群)報告較高的GSH、糖原和磷脂相關代謝物濃度;HPV陽性女性在所有陰道微生物群狀態下胺類、脂類和肽類濃度低於HPV陰性女性;高水平的生物胺和GSH創造的陰道氧化應激環境可能損害宿主對感染的反應 | [272] |
| 意大利博洛尼亞 | 79名女性:21名健康、20名BV、20名CT、18名VVC感染女性<br>橫斷面研究<br>使用16S rRNA MiSeq測序進行微生物分析,1H-NMR進行代謝組學分析 | 健康女性的陰道微生物群以卷曲乳酸桿菌 [L. crispatus] 主導;CT感染女性報告乳酸桿菌低豐度,陰道阿托波菌 [A. vaginae]、糞桿菌 [Faecalibacterium]、大球菌 [Megasphaera]、羅氏菌 [Roseburia] 豐度高;BV和VVC感染女性報告乳酸桿菌低豐度和BVAB高豐度;陰道菌群失調(BV、VVC、CT)條件下二甲胺減少、三甲胺水平增加;健康女性產生較多的乳酸和支鏈氨基酸(即纈氨酸、亮氨酸、異亮氨酸);BV感染女性報告生物胺和短鏈有機酸增加;VVC感染女性報告較高的葡萄糖水平,可能減少卷曲乳酸桿菌 [L. crispatus] 豐度並促進念珠菌的毒力 | [24] |
| 美國密蘇里州(聖路易斯) | 255 名女性:42 名假絲酵母菌定植和 255名女性:42名念珠菌定殖、213名非念珠菌定殖<br>包括黑人和白人女性,具正常、中間和BV型陰道微生物群<br>巢式橫斷面研究<br>使用16S rRNA qPCR進行微生物分析<br>乳酸桿菌對念珠菌體外生長的抑制試驗 | 20%(52/255)、39%(99/255)和38%(98/255)的女性分別報告卷曲乳酸桿菌 [L. crispatus]、陰道乳桿菌 [L. iners] 和非乳酸桿菌主導的陰道微生物群;以陰道乳桿菌 [L. iners] 主導的陰道微生物群比以卷曲乳酸桿菌 [L. crispatus] 主導的更容易有念珠菌定殖;卷曲乳酸桿菌 [L. crispatus] 的無細胞上清液pH值較低(質子化乳酸水平高),相較於陰道乳桿菌 [L. iners] 更有效抑制念珠菌定殖 | [273] |
| 盧安達 基加利 | 68名高風險BV或TV患者:僅55名主動尋求治療<br>受試者接受7天500毫克口服甲硝唑治療<br>使用16S rRNA HiSeq測序和BactQuant 16S基因定量PCR進行微生物分析 | 甲硝唑治療後BV治癒率僅達54.5%;治療後BV厭氧菌豐度適度減少(16.4%的患者BV群體減少50%);乳酸桿菌總豐度增加,其中陰道乳桿菌 [L. iners] 在治療後(成功和失敗)錄得最高豐度;高豐度的病原共生菌和陰道加德納菌 [G. vaginalis] 與治療失敗的可能性相關,可能由於生物膜形成 | [274] |
CT: 衣原體(Chlamydia trachomatis)
RVVC: 反覆性外陰陰道念珠菌病(Recurrent Vulvovaginal Candidiasis)
VVC: 外陰陰道念珠菌病(Vulvovaginal Candidiasis)
TV: 陰道毛滴蟲(Trichomonas vaginalis)
BV-VVC: 陰道細菌性病和外陰陰道念珠菌病的共感染(Co-infection of BV and VVC)
BVAB: 陰道細菌性病相關細菌(BV-associated Bacteria)
CSTs: 社群狀態型(Community State Types)
IP-10: 干擾素-γ誘導蛋白-10(化學趨化因子)(Interferon-γ induced protein-10, Chemokine)
ITS: 內部轉錄間隔區(Internal Transcribed Spacer)
OTUs: 操作性分類單元(Operational Taxonomic Units)
PTB: 早產(Preterm Birth)
T1D: 一型糖尿病(Type-I Diabetes)
白色念珠菌(Candida albicans)
白色念珠菌(Candida albicans)是陰道的主要定殖者,常從外陰陰道念珠菌病(VVC)感染女性中分離出來 [72, 73]。外陰陰道念珠菌病在一生中至少影響75%的女性 [72],而首次VVC發作的女性中約有5-10%會發展成復發性外陰陰道念珠菌病(RVVC,每年超過四次發作) [74]。作為陰道中最常見的居民之一,白色念珠菌(C. albicans)經常被證明與乳酸桿菌共同定殖於陰道 [75]。此外,非白色念珠菌(NCAC)物種,如熱帶念珠菌(Candida tropicalis)、光滑念珠菌(C. glabrata)、克魯斯念珠菌(C. krusei)、都柏林念珠菌(C. dubliniensis)和平滑念珠菌(C. parapsilosis),也常在RVVC感染女性中被觀察到 [76–79]。VVC和復發性VVC患者報告的非特異性症狀包括外陰紅斑、瘙癢、性交疼痛、灼熱感、白色塊狀分泌物和酸痛 [72, 80]。雖然VVC不危及生命,但未解決的VVC會影響患者的生活質量,例如心理健康、社交生活、性關係和工作生活 [74, 81]。
白色念珠菌(Candida albicans)是一種多形性酵母菌,能在有利條件下從酵母形態轉變為菌絲形態 [82, 83]。關於白色念珠菌如何從單純的定殖者轉變為病原菌的一些合理解釋包括陰道菌群失調、毒力因子表達(如菌絲和生物膜形成)以及產生蛋白水解酶(如分泌的天門冬氨酸蛋白酶,SAPs),這些導致陰道免疫毒性 [84]。Swidsinski等人證明,VVC患者的上皮內病變中含有白色念珠菌(C. albicans)菌絲,並伴隨陰道加德納菌(G. vaginalis)和陰道乳桿菌(L. iners)的共同入侵 [85]。這是最有力的證據之一,顯示白色念珠菌的形態可塑性(從酵母到菌絲的形成)以及BV相關細菌(BVAB)的存在可能導致症狀性VVC。此外,陰道微生物群的破壞(如乳酸菌群體減少)可能促進念珠菌屬物種入侵陰道上皮細胞的能力 [18]。在突破陰道上皮細胞後,白色念珠菌的假菌絲和菌絲通過級聯激活誘導上皮細胞的NLRP3炎症體受體,最終引發嚴重的陰道炎症 [86]。在所有陰道微生物群和真菌群研究中,白色念珠菌(C. albicans)仍是VVC最常描述的致病因子 [87]。VVC的顯著特徵是由念珠菌屬物種引起的陰道菌群失調和陰道黏膜炎症 [85]。此外,陰道真菌群的變化被證明與糖尿病、懷孕、免疫缺陷-過敏性鼻炎和復發性外陰陰道念珠菌病(RVVC)狀態相關 [88, 89]。正如討論所述,微生物群與真菌群的相互作用可能通過它們之間的短暫或持續相互作用,促進女性VVC的發展。探索這些相互作用並尋找潛在的微生物干預措施對於預防和治療女性VVC至關重要。
細菌性陰道病(BV)
細菌性陰道病(BV)是育齡婦女中最常見的陰道炎症,其特徵是陰道微生物群組成從以乳酸桿菌為主轉變為多微生物群落 [24, 90]。根據Peebles等人,全球七個地區23-29%的女性人口感染了BV,這造成了每年37億至61億美元的巨大經濟負擔 [91]。細菌性陰道病可通過Amsel標準、革蘭氏染色、Nugent評分和分子檢測診斷 [40, 92]。它通常伴隨大量陰道加德納菌(G. vaginalis)、普雷沃氏菌屬(Prevotella)、陰道阿托波菌(A. vaginae)、血鏈球菌屬(Sneathia)和其他BVAB,這是由於陰道微生物群失調所致 [93, 94]。BV經常與HIV感染、流產、盆腔炎性疾病、早產、產後子宮內膜炎和性傳播感染(STIs)獲得的風險升高相關 [90, 95–97]。此外,BV最終會對女性造成顯著的心理社會壓力。Bilardi等人 [98] 證明,復發性BV女性經常在日常生活中體驗到尷尬、自卑和挫折感。
可以設想,乳酸桿菌產生的細菌素和乳酸抑制了陰道中BVAB的過度增殖 [99]。然而,當陰道菌群失調發生時,以乳酸桿菌為主的陰道微生物群被陰道加德納菌(Gardnerella)和其他BVAB的過度生長所取代 [100]。近期研究表明,BVAB(如陰道加德納菌和陰道阿托波菌)之間的協同作用顯著增強了BV的嚴重性,增加了細菌負擔 [101, 102]。BV的另一個重要特徵是以陰道加德納菌為主的多微生物生物膜形成,而其他共同定殖的BVAB被證明增強了陰道加德納菌生長的生物膜厚度 [85, 103–105]。多項研究還表明,與乳酸桿菌數量減少相關的BV陰道微生物群增加了其他STIs的發病率 [106–108]。Cone [109] 推斷,以乳酸桿菌為主的微生物群通過強烈酸化陰道環境和降低炎症細胞因子來減少STIs的傳播。多項研究也一致表明,乳酸桿菌的存在通過乳酸顯著降低了沙眼衣原體(C. trachomatis)的毒力 [54, 110, 111]。
性傳播感染(STIs)
性傳播感染(STIs),如衣原體感染(主要由沙眼衣原體 C. trachomatis 引起)、淋病(淋病奈瑟氏菌 Neisseria gonorrhoeae)、滴蟲病(陰道滴蟲 Trichomonas vaginalis)和梅毒(蒼白螺旋體 Treponema pallidum),常在女性中引發嚴重的宮頸炎、尿道炎、陰道炎和生殖器潰瘍 [112–114]。根據世界衛生組織(WHO),全球每年STIs的估計數為3.764億(衣原體感染:1.272億;淋病:8690萬;梅毒:630萬;滴蟲病:1.56億) [112]。通常,STIs可通過短期抗生素治療治癒。然而,若不治療,STIs可能傳染給他人並引發流行病 [115]。這些STIs通常與女性宮頸癌、不孕、早產和盆腔炎性疾病的高風險相關 [114, 116, 117]。多項研究一致表明,破壞的或與BV相關的陰道微生物群(乳酸桿菌豐度低)增加了STIs的發病率 [106–108, 118–120]。此外,STIs的發生與HIV感染的高風險相關。Galvin和Cohen [121] 表明,STIs能夠破壞陰道黏膜層和免疫穩態,導致HIV脫落增加 [121]。同時,無症狀沙眼衣原體感染在感染者中常被漏診和未治療 [122]。富含乳酸桿菌的平衡陰道微生物群能夠調節陰道上皮細胞增殖和D-乳酸產生,隨後減少沙眼衣原體基本體進入上皮細胞 [54]。因此,這些研究強調了陰道穩態在提供對抗陰道感染的天然屏障的重要性。
尿路感染(UTIs)
陰道還是女性尿路感染(UTIs)致病菌的儲存庫 [123]。引起UTIs的最常見病原菌包括大腸桿菌(Escherichia coli)、肺炎克雷伯菌(Klebsiella pneumoniae)、表皮葡萄球菌(Staphylococcus epidermidis)、無乳鏈球菌(Streptococcus agalactiae,B組鏈球菌)、糞腸球菌(Enterococcus faecalis)、奇異變形桿菌(Proteus mirabilis)和綠膿桿菌(Pseudomonas aeruginosa) [124–126]。雖然UTIs可通過抗生素治癒,但嚴重併發症,包括腎盂腎炎、血尿和慢性腎病(CKD),可能導致永久性腎損傷 [127, 128]。研究表明,病原菌如陰道加德納菌(Gardnerella)、普雷沃氏菌(Prevotella)和脲原體(Ureaplasma)可能從陰道通過尿道和膀胱上升至尿路引起感染 [129–131]。與以乳酸桿菌為主的陰道微生物群相比,陰道菌群失調被證明增加了UTIs獲得的風險 [123, 132]。事實上,將小鼠陰道暴露於陰道加德納菌(G. vaginalis)引發了由大腸桿菌(E. coli)引起的復發性UTIs [133]。因此,維持陰道穩態可以抑制尿路中致病菌的發病。
中毒性休克綜合症(TSS)
另一種困擾育齡婦女的嚴重疾病是中毒性休克綜合症(TSS),與陰道中定殖的產生TSS毒素(TSST-1)的金黃色葡萄球菌(S. aureus)相關 [134]。眾所周知,TSST-1在中性pH值(即pH 6.5-7.0)下產生,這種條件在疾病狀態的陰道中經常報導 [135]。多項研究表明,使用月經杯、衛生棉條和避孕隔膜會破壞以乳酸桿菌為主的陰道微生物群,並增強金黃色葡萄球菌(S. aureus)的生長和TSST-1的產生 [136–138]。TSST-1的過量產生可能導致女性嚴重併發症,如器官衰竭、全身炎症和死亡 [139]。總之,陰道菌群失調可能導致陰道中乳酸菌保護作用的喪失,並增加從陰道上升的致病菌風險,最終導致UTIs。
陰道微生物群的平衡與失調
平衡良好和破壞的陰道微生物群與健康和疾病狀態的陰道密切相關。除了宿主對BV、STIs、VVC和UTIs的易感性外,陰道微生物群的破壞積極剝奪了乳酸桿菌對陰道中機會性病原菌的有益功能。進一步探索具有整體研究設計(如多樣化人群、種族和地理區域)可能有助於開發預測標誌物,用於診斷破壞的陰道微生物群。隨後需要通過使用生物治療劑(如乳酸桿菌)來改善和恢復陰道微生物群至非疾病狀態,以降低這些陰道感染的風險。
乳酸桿菌在控制陰道病原菌中的潛力
乳酸菌是一類多樣細菌的代表性微生物,其特徵為革蘭氏陽性、微需氧、耐酸、不產孢子並能產生乳酸 [140, 141]。用作益生菌的主要乳酸菌屬包括乳酸桿菌(Lactobacillus)、雙歧桿菌(Bifidobacterium)、鏈球菌(Streptococcus)、腸球菌(Enterococcus)和片球菌(Pediococcus) [142, 143]。美國食品藥品監督管理局(FDA)授予乳酸的普遍認為安全(GRAS)地位,使其在食品、乳製品和製藥行業中得到廣泛應用 [144, 145]。例如,德氏乳桿菌保加利亞亞種(Lactobacillus delbrueckii subsp. bulgaricus)與嗜熱鏈球菌(Streptococcus thermophilus)一起被用作製造酸奶和奶酪的發酵劑 [146, 147]。根據Reid等人,適量給予益生菌乳酸桿菌能夠通過恢復微生物和宿主免疫穩態為宿主帶來健康益處 [148]。
越來越多的研究闡明了乳酸桿菌對胃腸道、口腔、陰道和表皮層中病原菌的基本益生菌效應 [149–152]。嗜酸乳桿菌(Lactobacillus acidophilus)KS400已被證明通過發酵產生細菌素,抑制尿生殖道病原菌如陰道加德納菌(G. vaginalis)、無乳鏈球菌(S. agalactiae)和綠膿桿菌(P. aeruginosa)的生長 [153]。此外,來自陰道的鼠李糖乳桿菌(L. rhamnosus)(Lactocin 160)的細菌素能夠通過破壞病原菌的化學滲透勢在陰道加德納菌(G. vaginalis)的細胞膜上產生瞬時孔隙 [154]。多項研究還表明,好氧性陰道炎(AV)引起的病原菌,如大腸桿菌(E. coli)、糞腸球菌(E. faecalis)、金黃色葡萄球菌(S. aureus)、表皮葡萄球菌(S. epidermidis)和無乳鏈球菌(S. agalactiae),通常駐留在陰道中並誘發炎症性陰道炎 [155, 156]。長期使用抗菌藥物治療陰道炎可能導致耐藥性的發展 [157, 158]。因此,基於益生菌乳酸桿菌的方法作為傳統抗菌治療的替代方案正在被廣泛研究。根據Bertuccini等人 [159],鼠李糖乳桿菌(L. rhamnosus)HN001和嗜酸乳桿菌(L. acidophilus)GLA-14能夠顯著抑制陰道加德納菌(G. vaginalis)、陰道阿托波菌(A. vaginae)、金黃色葡萄球菌(S. aureus)和大腸桿菌(E. coli)的生長。為了闡明乳酸桿菌引入陰道微生物群的效果,一項研究表明,口服混合嗜酸乳桿菌(L. acidophilus)La-14和鼠李糖乳桿菌(L. rhamnosus)HN001從第7天和第14天開始顯著增加了陰道中鼠李糖乳桿菌和嗜酸乳桿菌的豐度 [160]。在一項類似研究中,口服給予益生菌配方(嗜酸乳桿菌 L. acidophilus PBS066和羅伊氏乳桿菌 L. reuteri PBS072)以及(植物乳桿菌 L. plantarum PBS067、鼠李糖乳桿菌 L. rhamnosus PBS070和乳雙歧桿菌 B. lactis PBS075)與安慰劑對照組相比,從第7天開始顯著增加了陰道中乳酸桿菌和雙歧桿菌的豐度 [161]。除此之外,還報導多種乳酸桿菌菌株的培養上清液通過抑制黏附和菌絲相關基因的表達顯著抑制了白色念珠菌(C. albicans) [162]。諷刺的是,與SAPs相關的基因未受影響,因此表明這些蛋白酶在乳酸桿菌主導的陰道中白色念珠菌生存的重要性。觀察到的抗念珠菌活性部分歸因於細菌素、過氧化氫和乳酸的存在 [162]。此外,Li等人指出,卷曲乳酸桿菌(L. crispatus)和德氏乳桿菌(L. delbrueckii)在VVC Sprague-Dawley大鼠模型中與未治療對照組相比,能夠抑制60-70%的白色念珠菌(C. albicans) [163]。
乳酸桿菌干預已被證明在與抗菌藥物聯合治療和預防復發性感染中是有益的。採用這種方法的一項研究表明,口服多種乳酸桿菌(發酵乳桿菌 L. fermentum 57A、加氏乳桿菌 L. gasseri 57C和植物乳桿菌 L. plantarum 57B)與甲硝唑聯合給藥,顯著延長了BV(51%)和AV(71%)的復發時間,並維持了陰道pH的酸性 [164]。人們認為,耐膽汁酸的乳酸桿菌能夠在遷移到陰道腔之前增加腸道中乳酸桿菌的豐度 [148, 165]。然而,口服益生菌如何遷移並在陰道中占主導地位的確切機制仍存在爭議 [166, 167]。陰道內給予益生菌也被發明用於恢復破壞的陰道微生物群。Bohbot等人 [168] 報導,28天陰道內給予凍乾的卷曲乳酸桿菌(L. crispatus)IP 174178能夠降低復發率(20.5%),並與安慰劑對照組相比延長了BV復發的時間(28%)。此外,含有發酵乳桿菌(L. fermentum)LF15和植物乳桿菌(L. plantarum)LP01的陰道片劑通過抑制陰道加德納菌(G. vaginalis),恢復了陰道pH的酸性和Nugent評分低於7的閾值(平衡的陰道微生物群) [169]。鼠李糖乳桿菌(L. rhamnosus)BMX 54也已在BV患者中進行臨床測試,顯示在三個月給藥後能夠將陰道微生物群恢復到平衡狀態 [170]。此外,鼠李糖乳桿菌(L. rhamnosus)BMX 54還顯示其作為輔助治療的潛力,在6至9個月的治療後重塑陰道微生物群並減少BV復發 [171]。近期證據表明,間歇性應用陰道膠囊(含有嗜酸乳桿菌 L. acidophilus W70、短乳桿菌 L. brevis W63、瑞士乳桿菌 L. helveticus W74、植物乳桿菌 L. plantarum W21、唾液乳桿菌 L. salivarius W24和雙歧雙歧桿菌 Bifidobacterium bifidum W28)恢復了以乳酸桿菌為主的陰道微生物群,並與未治療對照組(每人年10.18)相比顯著降低了BV發病風險2.8倍 [172]。同時,使用乳酸桿菌還可以降低VVC復發率。例如,口服克黴唑和含有嗜酸乳桿菌(L. acidophilus)GLA-14和鼠李糖乳桿菌(L. rhamnosus)HN001以及牛乳鐵蛋白RCX的口服膠囊聯合給藥,與非乳酸桿菌給藥對照組相比,在三個月和六個月時分別顯著降低了VVC復發率58.4%和70.8% [173]。恢復陰道微生物群對於預防各種陰道感染及其復發率至關重要。根據Xie等人 [174],與傳統藥物治療相比,僅使用益生菌對抗VVC和BV的證據不足以推薦。
以乳酸桿菌為主的健康陰道生態系統有潛力保護宿主免受HIV和STIs的侵害 [20, 175]。根據McClelland等人,高豐度的BVAB與女性HIV感染風險相關 [108],可能是由於陰道pH值升高和產生抑制抗HIV免疫的酶 [176]。多項研究已進行體外和離體試驗,以確定乳酸桿菌在抑制BV相關細菌和HIV傳播的潛力 [177, 178]。從陰道分離的乳酸桿菌菌株產生的培養上清液已被證明能夠抑制人類宮頸陰道組織中的HIV-1型感染 [178]。在這項研究中,乳酸桿菌培養上清液被證明具有殺病毒作用,有助於減少宿主中病毒粒子的傳播 [178]。此外,加熱殺死的加氏乳桿菌(L. gasseri)也對TZM-bl細胞系上的HIV-1株X4感染性表現出高抑制活性(81.5%) [179]。在一項類似研究中,乾酪乳桿菌(L. casei)393(1×10⁴細胞/毫升)在30分鐘共孵育後能夠抑制HIV-1偽病毒(AD8、DH12和LA1),抑制範圍為60-70% [180]。最近,Palomino等人發現,乳酸桿菌對HIV-1感染的抑制作用與細胞外囊泡的存在相關,這些囊泡抑制HIV黏附和病毒進入目標細胞 [181]。前瞻性研究一致表明,破壞的陰道微生物群增加了女性HIV感染的風險 [23]。未來研究應優先闡明陰道菌群失調與HIV感染的機制,並發現益生菌乳酸桿菌作為HIV預防的有效干預措施。
總體而言,乳酸桿菌在預防陰道感染(如BV和VVC)方面顯示出令人期待的效果。使用益生菌乳酸桿菌來糾正陰道微生物群失衡的補充方法迫切需要,以減少抗菌藥物的使用。應進行更多關於益生菌乳酸桿菌對抗陰道感染效果的臨床試驗,以解決益生菌效果的異質性。
乳酸桿菌表面活性分子(SAMs)的潛力
許多潛在機制被提出負責乳酸桿菌的益生菌效應,包括競爭定殖、調節宿主免疫反應、促進有益微生物群的交叉餵養、產生和分泌乳糖酶、膽鹽水解酶、有機酸和抗菌化合物 [回顧於 [182, 183]]。與宿主-乳酸桿菌相互作用相關的益生菌特性被認為是由乳酸桿菌表面活性分子(SAMs)貢獻的 [184]。已報導支持益生菌作用的乳酸桿菌SAMs包括肽聚醣(PG)、細菌多醣、生物表面活性劑(BS)和壁酸(TA) [185, 186]。乳酸菌共有的核心SAMs包括脂壁酸、多醣、表面層相關蛋白(SLAPs)、黏蛋白結合蛋白(MUBs)和纖維連接蛋白結合蛋白 [187]。這些核心SAMs在乳酸菌黏附時調節宿主-微生物相互作用。事實上,已證明SAMs通過直接黏附於上皮細胞和黏膜層上的模式識別受體(PRRs)直接介導宿主生理反應 [187]。由於乳酸桿菌SAMs可能對調節陰道中的宿主-微生物相互作用很重要,應更加關注這些SAMs的研究,以開發新型基於SAMs的治療方法,作為當前可用治療方案的潛在替代品。
肽聚醣(PG)
肽聚醣(PG)是一種生物聚合物,由糖鏈組成,通過N-乙醯葡糖胺(GlcNAc)和N-乙醯胞壁酸(MurNAc)側鏈連接,形成革蘭氏陽性細菌(如乳酸桿菌和雙歧桿菌)的細胞表面 [188, 189]。通常,乳酸桿菌的細胞膜被PG網絡和其他生物聚合物包圍,即壁酸(TA)、S層蛋白和多醣 [189, 190]。
一般來說,STI病原菌如淋病奈瑟氏菌(N. gonorrhoeae)能夠通過抑制白細胞介素-12(IL-12)的產生來抑制宿主Th-1驅動的適應性免疫反應 [191]。有鑑於此,陰道內給予微囊化的IL-12能夠逆轉小鼠的免疫抑制,並促進淋病感染的清除 [191]。同時,乳酸桿菌PG表現出卓越的免疫調節活性,改善宿主先天免疫反應。例如,乾酪乳桿菌(L. casei)PG能夠通過Toll樣受體2(TLR2)和核苷酸結合寡聚化域2(NOD2)誘導小鼠腹腔巨噬細胞產生IL-12 [192]。此外,植物乳桿菌(L. plantarum)CAU1055 PG證明能夠通過抑制一氧化氮(NO)合酶、環氧合酶-2(COX-2)和細胞因子(TNF-α和白細胞介素-6)來緩解RAW264.7小鼠巨噬細胞中一氧化氮誘導的炎症 [193]。在一項類似研究中,嗜酸乳桿菌(L. acidophilus)衍生的PG也被報導在LPS誘導的RAW 264.7巨噬細胞上顯著降低NO合酶和COX-2水平 [194]。此外,陰道分離的卷曲乳酸桿菌(L. crispatus)PG能夠刺激朗格漢斯細胞(陰道上的抗原呈現樹突狀細胞)的CD207表達,並顯著降低HIV進入受體的表達 [195]。陰道上皮細胞中陰道微生物群和免疫系統的平衡對於預防陰道感染至關重要 [196]。PG在調節免疫穩態的潛在效果可以有效協助維持女性健康的陰道生態系統。除了報導的免疫調節活性外,短乳桿菌(L. brevis)PG還表現出對生殖器單純皰疹病毒-2(HSV-2)的強抗病毒活性 [197]。根據Mastromarino等人 [197],短乳桿菌(L. brevis)PG的抗病毒活性不受熱和蛋白酶處理影響,並仍以濃度依賴方式顯著抑制HSV-2複製。
脂壁酸(LTA)
乳酸桿菌PG通常被壁酸(TA)或脂壁酸(LTA)裝飾 [198]。脂壁酸由甘油-磷酸聚合作用生成,並與細胞膜結合 [199, 200]。與其他SAMs一起,LTA調節宿主的模式識別受體(PPRs)和若干信號通路,這些通路負責乳酸桿菌的益生菌和抗病原菌效果 [185]。消除人類陰道中的多微生物生物膜是阻礙細菌毒力並預防BV發病的一種策略 [201]。植物乳桿菌(L. plantarum)LTA通過減弱蔗糖分解阻礙了羥基磷灰石盤上變形鏈球菌(S. mutans)生物膜的形成 [35]。此外,植物乳桿菌(L. plantarum)LTA顯著抑制了人類牙本質切片上糞腸球菌(E. faecalis)生物膜的形成和預形成的生物膜,表明LTA可用作預防和治療糞腸球菌感染的措施 [202]。此外,植物乳桿菌(L. plantarum)LTA抑制了由奈氏放線菌(Actinomyces naeslundii)、唾液乳桿菌(L. salivarius)、糞腸球菌(E. faecalis)和變形鏈球菌(S. mutans)組成的多微生物生物膜在牙本質切片上的形成 [203]。除了抗黏附和抗生物膜特性外,乳酸桿菌LTA還具有免疫調節活性。例如,約氏乳桿菌(Lactobacillus johnsonii)La1和嗜酸乳桿菌(L. acidophilus)La10的LTA在脂多醣(LPS)或革蘭氏陰性細菌存在下,緩解了腸上皮細胞中促炎細胞因子(如TNF-α、IL-8和白細胞介素-5(ENA-78))的過度刺激 [204]。根據Ahn等人,來自植物乳桿菌(L. plantarum)K8的LTA也在LPS挑戰的THP-1細胞中調節了炎症細胞因子(TNF-α和IL-10)的產生 [205]。患有BV和性傳播疾病的患者通常與促炎細胞因子的過度刺激和中性粒細胞向陰道黏膜表面的募集相關 [119, 206]。因此,乳酸桿菌LTA的免疫調節活性可以減弱由病原菌引起的過度刺激和陰道炎症。
細菌多醣
細菌在細胞表面形成緊密連接的聚合物,並將其釋放到環境中作為胞外多醣(EPS)(鬆散未附著的黏液) [31, 207]。通過利用表面多醣模仿宿主的糖結構,致病菌能夠在定殖期間逃避宿主免疫系統 [208]。一般來說,細菌分泌的EPS對於宿主-微生物相互作用中的黏附和細胞識別至關重要 [209]。胞外多醣是高分子量、可生物降解的碳水化合物聚合物,根據其單醣成分分為同多醣或雜多醣 [回顧於 [210–212]]。過去十年中,乳酸菌的EPS因其抑制蠟樣芽孢桿菌(Bacillus cereus)產生的細菌毒素的能力而獲得了大量關注 [213]。乳酸桿菌EPS的產生受發酵期間培養條件和營養成分的調節 [214, 215]。例如,鼠李糖乳桿菌(L. rhamnosus)EPS的產生在與釀酒酵母(S. cerevisiae)共同發酵48小時後顯著增加了40-50%,這是由於EPS操縱子表達的上調增強了氨基酸生物合成、碳水化合物代謝和脂肪酸代謝 [216]。此外,五碳乳桿菌(Lactobacillus pentosus)EPS的產生受到用於發酵過程的不同碳源的強烈影響,例如葡萄糖增強了EPS的黏度,在牛奶生產中具有更好的增稠效果 [217]。類似研究還報導,在補充葡萄糖作為碳源的de Man, Rogosa和Sharpe(MRS)培養基中觀察到植物乳桿菌(L. plantarum)EPS的更高產量 [218]。培養基的不同碳源也顯著影響乳酸桿菌EPS的功能活性。作為證明,補充蔗糖的MRS顯著增加了植物乳桿菌(L. plantarum)LPC-1的EPS產量 [219]。然而,當使用葡萄糖作為碳源時,植物乳桿菌(L. plantarum)LPC-1報告了更高的抗氧化活性,與蔗糖相比 [219]。總體而言,影響EPS產生的兩個並存因素(乳酸桿菌菌株和碳源)導致了EPS不同的流變特性,這可能影響EPS的功能活性。
乳酸桿菌EPS的獨特理化特性有潛力為人類帶來健康益處,已報導其具有抗動脈粥樣硬化、抗癌、抗氧化、抗病毒、抗酵母、免疫調節和益生元特性 [220–224]。人類防禦素-2是由宿主上皮細胞分泌的抗菌肽,有助於調節陰道道的炎症和微生物群功能 [225]。相應地,卷曲乳酸桿菌(L. crispatus)L1 EPS強烈增強了陰道上皮VK2細胞產生人類防禦素-2蛋白(殺念珠菌效果)的能力,並通過競爭性排斥減少了白色念珠菌(C. albicans)的黏附(48%) [226]。同樣,鼠李糖乳桿菌(L. rhamnosus)GG EPS與多種念珠菌屬物種之間也觀察到競爭性排斥,如在VK2和人類支氣管Calu-3細胞系上分別顯著減少了白色念珠菌(C. albicans,30%)和光滑念珠菌(C. glabrata,25%)的黏附 [224]。可以設想,酵母到菌絲的轉換對白色念珠菌(C. albicans)的致病性和免疫病理學至關重要 [227]。Allonsius等人 [224] 進行的研究報導,鼠李糖乳桿菌(L. rhamnosus)GG的EPS將白色念珠菌(C. albicans)的菌絲形成抑制了40%,進一步證實了乳酸桿菌EPS的潛在抗念珠菌特性。細菌性陰道病以陰道上皮上多微生物生物膜的存在為特徵 [228]。植物乳桿菌(L. plantarum)WLPL04 EPS被報導顯著減少了大腸桿菌(E. coli)、綠膿桿菌(P. aeruginosa)、金黃色葡萄球菌(S. aureus)和沙門氏菌(Salmonella typhimurium)在HT-29細胞系上的黏附 [33],使其成為值得開發的潛在抗生物膜劑,用於更好的BV管理。
BV的發生與陰道環境中高氧化應激(如高水平的丙二醛(MDA)產生和低超氧化物歧化酶(SOD)活性)以及黏蛋白降解相關 [229, 230]。因此,陰道上皮的高抗氧化能力可能減少BV感染期間形成的氧化應激,並增強陰道免疫系統對抗病原菌至關重要。植物乳桿菌(L. plantarum)C88 EPS也被證明以劑量依賴方式表現出高抗氧化效果,通過降低MDA水平和提高SOD活性 [231]。此外,從瑞士乳桿菌(L. helveticus)KLDS1.8701提取的純EPS顯著改善了小鼠肝臟對氧化應激的抗氧化活性,通過降低SOD活性 [232]。除了抗氧化能力外,乳酸桿菌EPS還表現出改善細胞中降解黏蛋白屏障的能力。例如,植物乳桿菌(L. plantarum)EPS通過增加小鼠結腸中黏蛋白MUC2基因表達、緊密連接蛋白表達和杯狀細胞分化,促進黏膜癒合和保護 [233, 234]。事實上,黏蛋白已被證明能防止陰道病原菌的黏附,並促進乳酸菌在上皮細胞上的黏附 [25]。
EPS的益生元特性已被積極探索。一般來說,益生元可以從天然來源中提取,作為上皮細胞的能量來源,並刺激腸道中有益細菌的生長 [142]。一個化合物被認為是“益生元”的一般要求包括能夠抵抗胃腸道酶和小腸吸收,以及通過發酵刺激有益細菌的代謝活動的能力 [212]。Sims等人 [235] 表明,利用益生元寡糖如β-葡聚醣、菊粉和果寡糖刺激了益生菌乳酸菌的生長,表明益生元和益生菌的組合可以為宿主提供健康益處。短乳桿菌(L. brevis)ED25的葡聚醣EPS被證明增加了食品中益生菌鼠李糖乳桿菌(L. rhamnosus)GG的保質期,並提高了鼠李糖乳桿菌(L. rhamnosus)GG的存活率 [236]。來自益生菌EPS的多醣被認為通過細菌間的交叉對話在腸道表面提升正常菌群的豐度 [237]。可以推斷,類似的相互作用可能在陰道環境中的有益細菌中觀察到。
生物表面活性劑(BS)
生物表面活性劑(BS),也稱為生物乳化劑,是主要由微生物合成的兩親性活性化合物 [238]。這些兩親性分子賦予微生物通過乳化降低水溶液之間表面和界面張力的能力 [239]。生物BS可分為低分子量表面活性劑(如糖脂和脂肽)和高分子量表面活性劑(如糖蛋白複合物、脂多醣和脂蛋白) [240]。除了在農業、動物飼料、化妝品、食品和油工業中的重要作用外,BS最近因其生物修復潛力而引起科學界的關注 [241, 242]。然而,乳酸桿菌BS的功能活性仍未被充分研究 [240]。Mouafo等人表明,乳酸桿菌BS的產生取決於發酵碳源的選擇。來自甘蔗和甘油的碳源相較於MRS肉湯有效增加了BS的產量 [243]。
生物表面活性劑被報導通過改變微生物附著的表面化學性質表現出抗黏附和抗菌特性 [182]。槐糖脂是一種通常由非致病性酵母Starmerella bombicola產生的糖脂BS [244]。該化合物已被證明能夠抑制白色念珠菌(C. albicans)生物膜的形成,並破壞預形成的白色念珠菌生物膜 [244]。令人驚訝的是,Haque等人 [244] 還發現,槐糖脂與抗真菌藥物的組合在抑制白色念珠菌方面高效,治療後未觀察到白色念珠菌菌絲和生物膜複雜網絡。對於乳酸桿菌產生的BS,最近報導嗜酸乳桿菌(L. acidophilus)ATCC 4356、德氏乳桿菌(Lactobacillus debrueckii)ATCC 9645和副乾酪乳桿菌(Lactobacillus paracasei)11的BS顯著減少了陰道病原菌白色念珠菌(C. albicans)的生物膜形成,減少幅度為40-50% [245]。此外,來自短乳桿菌(L. brevis)CV8LAC的BS被報導在矽酮彈性盤上有效抑制24小時、48小時和72小時的白色念珠菌(C. albicans)生物膜形成(約90%) [246]。除了對白色念珠菌生物膜的抑制外,詹氏乳桿菌(L. jensenii)P6A和加氏乳桿菌(L. gasseri)P65的BS還表現出對多種尿生殖道病原菌(如大腸桿菌 E. coli、肺炎克雷伯菌 Klebsiella pneumoniae、腐生葡萄球菌 Staphylococcus saprophyticus 和產氣腸桿菌 Enterobacter aerogenes)的強抗菌和抗生物膜活性 [247]。此外,粗製副乾酪乳桿菌(L. paracasei)BS抑制了化膿鏈球菌(Streptococcus pyogenes)、表皮葡萄球菌(S. epidermidis)、大腸桿菌(E. coli)、綠膿桿菌(P. aeruginosa)、金黃色葡萄球菌(S. aureus)和無乳鏈球菌(S. agalactiae) [248]。Gudiña等人 [248] 發現,副乾酪乳桿菌(L. paracasei)BS在pH鹼化(pH 6至10)和熱處理(60°C)後仍高度穩定。此外,通過酸性製備提取的粗製副乾酪乳桿菌BS也大大增強了抗菌活性 [248]。多項研究還進行了識別乳酸桿菌BS對其他陰道和尿路病原菌效果的研究。根據Spurbeck和Arvidson [249],加氏乳桿菌(L. gasseri)33323 BS通過阻斷上皮細胞上的細胞外基質成分纖維連接蛋白,對性傳播病原菌淋病奈瑟氏菌(Neisseria gonorrhoeae)表現出抗黏附活性。來自卷曲乳酸桿菌(L. crispatus)的生物表面活性劑也在兩個時間點(即7分鐘和60分鐘)孵育後顯著抑制了淋病奈瑟氏菌(N. gonorrhoeae)的生長(>50%) [250]。Jiang等人報導,瑞士乳桿菌(L. helveticus)27170 BS對金黃色葡萄球菌(S. aureus)的抗黏附活性機制與破壞金黃色葡萄球菌中自誘導物-2信號(群體感應分子)相關 [251]。此外,Satpute等人揭示,嗜酸乳桿菌(L. acidophilus)BS能夠通過抗黏附機制減少醫療植入物聚二甲基矽氧烷(PDMS)表面上的大腸桿菌(E. coli)、金黃色葡萄球菌(S. aureus)、尋常變形桿菌(P. vulgaris)、枯草桿菌(B. subtilis)和惡臭假單胞菌(P. putida)的生物膜 [252]。最近,來自卷曲乳酸桿菌(L. crispatus)BC1的BS也在人類宮頸癌HeLa細胞系上通過排斥機制表現出顯著的體外抗黏附活性對抗白色念珠菌(C. albicans),並在小鼠中通過減少白色念珠菌引起的白細胞流入(即防止黏膜損傷)表現出體內免疫調節活性 [253]。根據這些發現,可以設想乳酸桿菌BS的作用機制涉及黏附中斷而非殺死入侵病原菌。
乳酸桿菌SAMs應用的挑戰
儘管有大量證據表明乳酸桿菌SAMs可能有益於人類,但其實施使用仍不明朗且具有挑戰性。其中一個挑戰是其生產所需的成本。由於其提取通常受到低產量的阻礙,優化生長培養基組成和提取方法至關重要 [210, 215, 254]。此外,碳源類型和pH值等其他因素也顯著影響EPS結構和產量 [255]。因此,SAMs的大規模生產通常需要額外的努力,可能耗時且成本效益低。此外,由於SAMs結構根據培養基組成的波動性質,SAMs在大規模工業化中的採用仍不明確。為了降低生產乳酸桿菌SAMs發酵的高成本,可以使用富含碳的農業廢物,如麩皮、甘蔗和甜菜糖蜜,作為替代培養基 [256]。利用低成本農業廢物基培養基可能減少大規模發酵過程中的高成本投入,並滿足未來乳酸桿菌SAMs的高市場需求。此外,通過確定最大產量的最經濟培養基組成,可以降低乳酸桿菌SAMs的生產成本 [215]。例如,通過配方調整和生產可能性曲線(PPC)進行的經濟建模,用於評估嗜酸乳桿菌(L. acidophilus)EPS生產的碳源,以確定最佳培養基組成和最佳生產集(OPS) [215]。根據Lin等人 [215],使用MRS-營養肉湯培養基生產嗜酸乳桿菌(L. acidophilus)EPS的總成本與僅使用MRS相比降低了30%(每升培養物7.5美元/公斤,相較於11.0美元/公斤)。此外,統計設計也是一種重要的方法,可用於優化培養基組成以實現乳酸桿菌SAMs的最大產量。最適合SAMs(如生物表面活性劑)生產的統計設計包括因子設計和響應面法(RSM) [257]。事實上,因子設計如Plackett-Burman設計(PBD)已被用於通過統計建模修改單因素和多因素(如碳源和氮源類型)來優化鼠李糖乳桿菌(L. rhamnosus)EPS生產的成本效益培養基 [254]。同時,RSM如中心複合設計(CCD)是一種備受讚譽的統計設計,用於分析和評估植物乳桿菌(L. plantarum)EPS生產增加的生長動力學參數 [218]。簡而言之,使用經濟建模和統計設計允許選擇影響乳酸桿菌SAMs生產的關鍵配方,最終可能降低SAMs生產的總體成本。此外,通過使用基因工程改造的SAMs生產乳酸桿菌菌株,可以改善從乳酸桿菌中回收SAMs。例如,Li等人 [258] 表明,通過重新路由EPS生產所需的NADH代謝途徑,可以將乾酪乳桿菌(L. casei)LC2W的EPS量增加46%。然而,使用基因工程改造的乳酸桿菌可能引起公眾的安全擔憂。通過在給藥前進行仔細的實驗檢查,可以解決潛在風險和安全問題 [259]。雖然已在體外進行了大量研究,但乳酸桿菌SAMs有效預防陰道感染的體內測試仍未充分研究。然而,異體免疫反應使得將健康陰道微生物群重建為以乳酸桿菌為主的微環境具有挑戰性。因此,需要個性化治療陰道感染的方法來宣稱乳酸桿菌的有益效果 [260]。此外,陰道感染的高復發率通常表明抗菌藥物在長期治療中的無效性。通過使用乳酸桿菌及其潛在衍生物(即SAMs),可以實現平衡陰道微生物群的恢復。未來研究應專注於創建經濟上可行的方法,用於大規模生成乳酸桿菌SAMs,以解決生產瓶頸並作為人類陰道感染的潛在治療方法。
結論
人類陰道中陰道微生物群和真菌群的存在塑造了陰道生態系統的健康和疾病狀態。在過去十年中,陰道微生物群分析已被廣泛研究。許多研究報導,健康的陰道CSTs通常以乳酸菌(即乳酸桿菌)為主,厭氧菌多樣性低,並具有平衡的陰道免疫系統(例如促炎和抗炎細胞因子)。宿主易感性和遺傳因素已被證明會改變陰道微生物組成。因此,破壞的陰道生態系統通常導致疾病狀態的CST和症狀性陰道炎。同時,乳酸桿菌已顯示在腸道和陰道中具有免疫調節和恢復健康微生物群的潛在健康益處。儘管在免疫缺陷患者中報導了罕見的乳酸桿菌菌血症,但其在減少陰道感染復發率和預防陰道獲得性感染方面的有益效果已得到充分證實。因此,應投資開發其他來自益生菌的潛在治療方法,以定位益生菌在免疫缺陷患者中的有前景的益處。
將乳酸桿菌用作預防措施似乎是一種長期的有益方法。正如本綜述討論的,乳酸桿菌衍生物(即SAMs)可以通過恢復原生微生物群及其抗生物膜能力作為陰道感染的預防措施。在BV患者中成功恢復以乳酸桿菌為主的組成被報導,復發率較低,同時與BV相關的細菌如陰道加德納菌(Gardnerella)、普雷沃氏菌(Prevotella)、大球菌(Megasphaera)、棒桿菌科(Coriobacteriaceae)和阿托波菌(Atopobium)顯著減少 [261]。乳酸桿菌SAMs對抗陰道病原菌的有益效果包括抗生物膜、抗氧化、抗病毒、病原菌抑制和免疫調節,被認為直接參與人類宿主與陰道微生物群之間的相互作用。考慮到乳酸桿菌SAMs顯著抑制陰道病原菌體外生長的能力,進一步研究應針對其在體內模型中的機制。這將是一個有價值的工具,有助於理解乳酸桿菌及其衍生物在調節陰道黏膜屏障對抗入侵病原菌中的作用。關於潛在乳酸桿菌SAMs及其各自機制知識的新證據將大大促進益生元和抗菌劑的開發,旨在預防和治療陰道疾病,如BV、STIs和VVC。
本文翻譯自論文Jeng, W. Y. C., Chew, S. Y., & Than, L. T. L. (2020). Vaginal microbiota and the potential of Lactobacillus derivatives in maintaining vaginal health. Microbial Cell Factories, 19, 203. doi: 10.1186/s12934-020-01464-4
參考文獻:
1.Lloyd-Price J, Mahurkar A, Rahnavard G, Crabtree J, Orvis J, Hall AB, et al. Strains, functions and dynamics in the expanded Human Microbiome Project. Nature. 2017;550:61–6. doi: 10.1038/nature23889. [DOI] [PMC free article] [PubMed] [Google Scholar]
2.Proctor LM, Creasy HH, Fettweis JM, Lloyd-Price J, Mahurkar A, Zhou W, et al. The integrative Human Microbiome Project. Nature. 2019;569:641–8. doi: 10.1038/d41586-019-01654-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
3.Turnbaugh PJ, Ley RE, Hamady M, Fraser-Liggett CM, Knight R, Gordon JI. The Human Microbiome Project. Nature. 2007;449:804–10. doi: 10.1038/nature06244. [DOI] [PMC free article] [PubMed] [Google Scholar]
4.Cho I, Blaser MJ. The human microbiome: at the interface of health and disease. Nat Rev Genet. 2012;13:260–70. doi: 10.1038/nrg3182. [DOI] [PMC free article] [PubMed] [Google Scholar]
5.Smith SB, Ravel J. The vaginal microbiota, host defence and reproductive physiology. J Physiol. 2017;595:451–63. doi: 10.1113/JP271694. [DOI] [PMC free article] [PubMed] [Google Scholar]
6.Gajer P, Brotman RM, Bai G, Sakamoto J, Schütte UME, Zhong X, et al. Temporal dynamics of the human vaginal microbiota. Sci Transl Med. 2012;4:132ra52. doi: 10.1126/scitranslmed.3003605. [DOI] [PMC free article] [PubMed] [Google Scholar]
7.Fredricks DN. Molecular methods to describe the spectrum and dynamics of the vaginal microbiota. Anaerobe. 2011;17:191–5. doi: 10.1016/j.anaerobe.2011.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
8.Franzosa EA, Hsu T, Sirota-Madi A, Shafquat A, Abu-Ali G, Morgan XC, et al. Sequencing and beyond: integrating molecular ‘omics’ for microbial community profiling. Nat Rev Microbiol. 2015;13:360–72. doi: 10.1038/nrmicro3451. [DOI] [PMC free article] [PubMed] [Google Scholar]
9.Johnson JS, Spakowicz DJ, Hong B-Y, Petersen LM, Demkowicz P, Chen L, et al. Evaluation of 16S rRNA gene sequencing for species and strain-level microbiome analysis. Nat Commun. 2019;10:5029. doi: 10.1038/s41467-019-13036-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
10.Ravel J, Gajer P, Abdo Z, Schneider GM, Koenig SSK, McCulle SL, et al. Vaginal microbiome of reproductive-age women. Proc Natl Acad Sci USA. 2011;108(Suppl 1):4680–7. doi: 10.1073/pnas.1002611107. [DOI] [PMC free article] [PubMed] [Google Scholar]
11.Ma B, Forney LJ, Ravel J. Vaginal microbiome: rethinking health and disease. Annu Rev Microbiol. 2012;66:371–89. doi: 10.1146/annurev-micro-092611-150157. [DOI] [PMC free article] [PubMed] [Google Scholar]
12.Hall RA, Noverr MC. Fungal interactions with the human host: exploring the spectrum of symbiosis. Curr Opin Microbiol. 2017;40:58–64. doi: 10.1016/j.mib.2017.10.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
13.Gow NAR, Hube B. Importance of the Candida albicans cell wall during commensalism and infection. Curr Opin Microbiol. 2012;15:406–12. doi: 10.1016/j.mib.2012.04.005. [DOI] [PubMed] [Google Scholar]
14.Zapata HJ, Quagliarello VJ. The microbiota and microbiome in aging: potential implications in health and age-related diseases. J Am Geriatr Soc. 2015;63:776–81. doi: 10.1111/jgs.13310. [DOI] [PMC free article] [PubMed] [Google Scholar]
15.Plummer EL, Vodstrcil LA, Fairley CK, Tabrizi SN, Garland SM, Law MG, et al. Sexual practices have a significant impact on the vaginal microbiota of women who have sex with women. Sci Rep. 2019;9:19749. doi: 10.1038/s41598-019-55929-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
16.Mulder M, Radjabzadeh D, Hassing RJ, Heeringa J, Uitterlinden AG, Kraaij R, et al. The effect of antimicrobial drug use on the composition of the genitourinary microbiota in an elderly population. BMC Microbiol. 2019;19:9. doi: 10.1186/s12866-018-1379-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
17.Hickey RJ, Zhou X, Settles ML, Erb J, Malone K, Hansmann MA, et al. Vaginal microbiota of adolescent girls prior to the onset of menarche resemble those of reproductive-age women. mBio. 2015;6:e00097-15. doi: 10.1128/mBio.00097-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
18.Bradford LL, Chibucos MC, Ma B, Bruno V, Ravel J. Vaginal Candida spp. genomes from women with vulvovaginal candidiasis. Pathog Dis. 2017;75:ftx061. doi: 10.1093/femspd/ftx061. [DOI] [PMC free article] [PubMed] [Google Scholar]
19.Mitra A, MacIntyre DA, Marchesi JR, Lee YS, Bennett PR, Kyrgiou M. The vaginal microbiota, human papillomavirus infection and cervical intraepithelial neoplasia: what do we know and where are we going next? Microbiome. 2016;4:58. doi: 10.1186/s40168-016-0203-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
20.van de Wijgert JHHM. The vaginal microbiome and sexually transmitted infections are interlinked: consequences for treatment and prevention. PLoS Med. 2017;14:e1002478. doi: 10.1371/journal.pmed.1002478. [DOI] [PMC free article] [PubMed] [Google Scholar]
21.Ziklo N, Vidgen ME, Taing K, Huston WM, Timms P. Dysbiosis of the vaginal microbiota and higher vaginal kynurenine/tryptophan ratio reveals an association with Chlamydia trachomatis genital infections. Front Cell Infect Microbiol. 2018;8:1. doi: 10.3389/fcimb.2018.00001. [DOI] [PMC free article] [PubMed] [Google Scholar]
22.Shannon B, Gajer P, Yi TJ, Ma B, Humphrys MS, Thomas-Pavanel J, et al. Distinct effects of the cervicovaginal microbiota and herpes simplex type 2 infection on female genital tract immunology. J Infect Dis. 2017;215:1366–75. doi: 10.1093/infdis/jix088. [DOI] [PMC free article] [PubMed] [Google Scholar]
23.Eastment MC, McClelland RS. Vaginal microbiota and susceptibility to HIV. AIDS. 2018;32:687–98. doi: 10.1097/QAD.0000000000001768. [DOI] [PMC free article] [PubMed] [Google Scholar]
24.Ceccarani C, Foschi C, Parolin C, D’Antuono A, Gaspari V, Consolandi C, et al. Diversity of vaginal microbiome and metabolome during genital infections. Sci Rep. 2019;9::14095. doi: 10.1038/s41598-019-50410-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
25.Amabebe E, Anumba DOC. The vaginal microenvironment: the physiologic role of lactobacilli. Front Med (Lausanne) 2018;5:181. doi: 10.3389/fmed.2018.00181. [DOI] [PMC free article] [PubMed] [Google Scholar]
26.O’Toole PW, Marchesi JR, Hill C. Next-generation probiotics: the spectrum from probiotics to live biotherapeutics. Nat Microbiol. 2017;2:17057. doi: 10.1038/nmicrobiol.2017.57. [DOI] [PubMed] [Google Scholar]
27.van Nood E, Vrieze A, Nieuwdorp M, Fuentes S, Zoetendal EG, de Vos WM, et al. Duodenal infusion of donor feces for recurrent Clostridium difficile. N Engl J Med. 2013;368:407–15. doi: 10.1056/NEJMoa1205037. [DOI] [PubMed] [Google Scholar]
28.Lev-Sagie A, Goldman-Wohl D, Cohen Y, Dori-Bachash M, Leshem A, Mor U, et al. Vaginal microbiome transplantation in women with intractable bacterial vaginosis. Nat Med. 2019;25:1500–4. doi: 10.1038/s41591-019-0600-6. [DOI] [PubMed] [Google Scholar]
29.Larsson P-G, Brandsborg E, Forsum U, Pendharkar S, Andersen KK, Nasic S, et al. Extended antimicrobial treatment of bacterial vaginosis combined with human lactobacilli to find the best treatment and minimize the risk of relapses. BMC Infect Dis. 2011;11:223. doi: 10.1186/1471-2334-11-223. [DOI] [PMC free article] [PubMed] [Google Scholar]
30.Anukam K, Osazuwa E, Ahonkhai I, Ngwu M, Osemene G, Bruce AW, et al. Augmentation of antimicrobial metronidazole therapy of bacterial vaginosis with oral probiotic Lactobacillus rhamnosus GR-1 and Lactobacillus reuteri RC-14: randomized, double-blind, placebo controlled trial. Microbes Infect. 2006;8:1450–4. doi: 10.1016/j.micinf.2006.01.003. [DOI] [PubMed] [Google Scholar]
31.Castro-Bravo N, Wells JM, Margolles A, Ruas-Madiedo P. Interactions of surface exopolysaccharides from Bifidobacterium and Lactobacillus within the intestinal environment. Front Microbiol. 2018;9:2426. doi: 10.3389/fmicb.2018.02426. [DOI] [PMC free article] [PubMed] [Google Scholar]
32.Kleerebezem M, Hols P, Bernard E, Rolain T, Zhou M, Siezen RJ, et al. The extracellular biology of the lactobacilli. FEMS Microbiol Rev. 2010;34:199–230. doi: 10.1111/j.1574-6976.2009.00208.x. [DOI] [PubMed] [Google Scholar]
33.Liu Z, Zhang Z, Qiu L, Zhang F, Xu X, Wei H, et al. Characterization and bioactivities of the exopolysaccharide from a probiotic strain of Lactobacillus plantarum WLPL04. J Dairy Sci. 2017;100:6895–905. doi: 10.3168/jds.2016-11944. [DOI] [PubMed] [Google Scholar]
34.Allonsius CN, Vandenheuvel D, Oerlemans EFM, Petrova MI, Donders GGG, Cos P, et al. Inhibition of Candida albicans morphogenesis by chitinase from Lactobacillus rhamnosus GG. Sci Rep. 2019;9:2900. doi: 10.1038/s41598-019-39625-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
35.Ahn KB, Baik JE, Park O-J, Yun C-H, Han SH. Lactobacillus plantarum lipoteichoic acid inhibits biofilm formation of Streptococcus mutans. PLoS One. 2018;13:e0192694. doi: 10.1371/journal.pone.0192694. [DOI] [PMC free article] [PubMed] [Google Scholar]
36.Brooks JP, Buck GA, Chen G, Diao L, Edwards DJ, Fettweis JM, et al. Changes in vaginal community state types reflect major shifts in the microbiome. Microb Ecol Health Dis. 2017;28:1303265. doi: 10.1080/16512235.2017.1303265. [DOI] [PMC free article] [PubMed] [Google Scholar]
37.Zheng N, Guo R, Yao Y, Jin M, Cheng Y, Ling Z. Lactobacillus iners is associated with vaginal dysbiosis in healthy pregnant women: a preliminary study. Biomed Res Int. 2019;2019:6079734. doi: 10.1155/2019/6079734. [DOI] [PMC free article] [PubMed] [Google Scholar]
38.Li F, Brix S, Wang Z, Chen C, Song L, Hao L, et al. The metagenome of the female upper reproductive tract. Gigascience. 2018;7:giy107. doi: 10.1093/gigascience/giy107. [DOI] [PMC free article] [PubMed] [Google Scholar]
39.Drell T, Lillsaar T, Tummeleht L, Simm J, Aaspõllu A, Väin E, et al. Characterization of the vaginal micro- and mycobiome in asymptomatic reproductive-age Estonian women. PLoS One. 2013;8:e54379. doi: 10.1371/journal.pone.0054379. [DOI] [PMC free article] [PubMed] [Google Scholar]
40.Kroon SJ, Ravel J, Huston WM. Cervicovaginal microbiota, women’s health, and reproductive outcomes. Fertil Steril. 2018;110:327–36. doi: 10.1016/j.fertnstert.2018.06.036. [DOI] [PubMed] [Google Scholar]
41.Younes JA, Lievens E, Hummelen R, van der Westen R, Reid G, Petrova MI. Women and their microbes: the unexpected friendship. Trends Microbiol. 2018;26:16–32. doi: 10.1016/j.tim.2017.07.008. [DOI] [PubMed] [Google Scholar]
42.Hickey RJ, Zhou X, Pierson JD, Ravel J, Forney LJ. Understanding vaginal microbiome complexity from an ecological perspective. Transl Res. 2012;160:267–82. doi: 10.1016/j.trsl.2012.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
43.Sabo MC, Balkus JE, Richardson BA, Srinivasan S, Kimani J, Anzala O, et al. Association between vaginal washing and vaginal bacterial concentrations. PLoS One. 2019;14:e0210825. doi: 10.1371/journal.pone.0210825. [DOI] [PMC free article] [PubMed] [Google Scholar]
44.Huang B, Fettweis JM, Brooks JP, Jefferson KK, Buck GA. The changing landscape of the vaginal microbiome. Clin Lab Med. 2014;34:747–61. doi: 10.1016/j.cll.2014.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
45.Doyle R, Gondwe A, Fan Y-M, Maleta K, Ashorn P, Klein N, et al. A Lactobacillus-deficient vaginal microbiota dominates postpartum women in rural Malawi. Appl Environ Microbiol. 2018;84:e02150-17. doi: 10.1128/AEM.02150-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
46.van de Wijgert JHHM, Borgdorff H, Verhelst R, Crucitti T, Francis S, Verstraelen H, et al. The vaginal microbiota: what have we learned after a decade of molecular characterization? PLoS One. 2014;9:e105998. doi: 10.1371/journal.pone.0105998. [DOI] [PMC free article] [PubMed] [Google Scholar]
47.DiGiulio DB, Callahan BJ, McMurdie PJ, Costello EK, Lyell DJ, Robaczewska A, et al. Temporal and spatial variation of the human microbiota during pregnancy. Proc Natl Acad Sci USA. 2015;112:11060–5. doi: 10.1073/pnas.1502875112. [DOI] [PMC free article] [PubMed] [Google Scholar]
48.De Seta F, Campisciano G, Zanotta N, Ricci G, Comar M. The vaginal community state types microbiome-immune network as key factor for bacterial vaginosis and aerobic vaginitis. Front Microbiol. 2019;10:2451. doi: 10.3389/fmicb.2019.02451. [DOI] [PMC free article] [PubMed] [Google Scholar]
49.Jakobsson T, Forsum U. Lactobacillus iners: a marker of changes in the vaginal flora? J Clin Microbiol. 2007;45:3145. doi: 10.1128/JCM.00558-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
50.Verstraelen H, Verhelst R, Claeys G, De Backer E, Temmerman M, Vaneechoutte M. Longitudinal analysis of the vaginal microflora in pregnancy suggests that L. crispatus promotes the stability of the normal vaginal microflora and that L. gasseri and/or L. iners are more conducive to the occurrence of abnormal vaginal microflora. BMC Microbiol. 2009;9:116. doi: 10.1186/1471-2180-9-116. [DOI] [PMC free article] [PubMed] [Google Scholar]
51.Breshears LM, Edwards VL, Ravel J, Peterson ML. Lactobacillus crispatus inhibits growth of Gardnerella vaginalis and Neisseria gonorrhoeae on a porcine vaginal mucosa model. BMC Microbiol. 2015;15:276. doi: 10.1186/s12866-015-0608-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
52.Fuochi V, Cardile V, Petronio Petronio G, Furneri PM. Biological properties and production of bacteriocins-like-inhibitory substances by Lactobacillus sp. strains from human vagina. J Appl Microbiol. 2019;126:1541–50. doi: 10.1111/jam.14164. [DOI] [PubMed] [Google Scholar]
53.France MT, Mendes-Soares H, Forney LJ. Genomic comparisons of Lactobacillus crispatus and Lactobacillus iners reveal potential ecological drivers of community composition in the vagina. Appl Environ Microbiol. 2016;82:7063–73. doi: 10.1128/AEM.02385-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
54.Edwards VL, Smith SB, McComb EJ, Tamarelle J, Ma B, Humphrys MS, et al. The cervicovaginal microbiota-host interaction modulates Chlamydia trachomatis infection. mBio. 2019;10:e01548-19. doi: 10.1128/mBio.01548-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
55.Witkin SS, Mendes-Soares H, Linhares IM, Jayaram A, Ledger WJ, Forney LJ. Influence of vaginal bacteria and D- and L-lactic acid isomers on vaginal extracellular matrix metalloproteinase inducer: implications for protection against upper genital tract infections. mBio. 2013;4:e00460-13. doi: 10.1128/mBio.00460-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
56.Borgdorff H, van der Veer C, van Houdt R, Alberts CJ, de Vries HJ, Bruisten SM, et al. The association between ethnicity and vaginal microbiota composition in Amsterdam, the Netherlands. PLoS One. 2017;12:e0181135. doi: 10.1371/journal.pone.0181135. [DOI] [PMC free article] [PubMed] [Google Scholar]
57.van de Wijgert JHHM, Verwijs MC, Gill AC, Borgdorff H, van der Veer C, Mayaud P. Pathobionts in the vaginal microbiota: individual participant data meta-analysis of three sequencing studies. Front Cell Infect Microbiol. 2020;10:129. doi: 10.3389/fcimb.2020.00129. [DOI] [PMC free article] [PubMed] [Google Scholar]
58.Kwak W, Han Y-H, Seol D, Kim H, Ahn H, Jeong M, et al. Complete genome of Lactobacillus iners KY using Flongle provides insight into the genetic background of optimal adaption to vaginal econiche. Front Microbiol. 2020;11:1048. doi: 10.3389/fmicb.2020.01048. [DOI] [PMC free article] [PubMed] [Google Scholar]
59.Chao X-P, Sun T-T, Wang S, Fan Q-B, Shi H-H, Zhu L, et al. Correlation between the diversity of vaginal microbiota and the risk of high-risk human papillomavirus infection. Int J Gynecol Cancer. 2019;29:28–34. doi: 10.1136/ijgc-2018-000032. [DOI] [PubMed] [Google Scholar]
60.Kyrgiou M, Mitra A, Moscicki A-B. Does the vaginal microbiota play a role in the development of cervical cancer? Transl Res. 2017;179:168–82. doi: 10.1016/j.trsl.2016.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
61.Lee JE, Lee S, Lee H, Song Y-M, Lee K, Han MJ, et al. Association of the vaginal microbiota with human papillomavirus infection in a Korean twin cohort. PLoS One. 2013;8:e63514. doi: 10.1371/journal.pone.0063514. [DOI] [PMC free article] [PubMed] [Google Scholar]
62.Kwasniewski W, Wolun-Cholewa M, Kotarski J, Warchol W, Kuzma D, Kwasniewska A, et al. Microbiota dysbiosis is associated with HPV-induced cervical carcinogenesis. Oncol Lett. 2018;16:7035–47. doi: 10.3892/ol.2018.9509. [DOI] [PMC free article] [PubMed] [Google Scholar]
63.Zhou Y, Wang L, Pei F, Ji M, Zhang F, Sun Y, et al. Patients with LR-HPV infection have a distinct vaginal microbiota in comparison with healthy controls. Front Cell Infect Microbiol. 2019;9:294. doi: 10.3389/fcimb.2019.00294. [DOI] [PMC free article] [PubMed] [Google Scholar]
64.Brusselaers N, Shrestha S, van de Wijgert J, Verstraelen H. Vaginal dysbiosis and the risk of human papillomavirus and cervical cancer: systematic review and meta-analysis. Am J Obstet Gynecol. 2019;221:9–18.e18. doi: 10.1016/j.ajog.2018.12.011. [DOI] [PubMed] [Google Scholar]
65.Mathema B, Cross E, Dun E, Park S, Bedell J, Slade B, et al. Prevalence of vaginal colonization by drug-resistant Candida species in college-age women with previous exposure to over-the-counter azole antifungals. Clin Infect Dis. 2001;33:e23-7. doi: 10.1086/322600. [DOI] [PubMed] [Google Scholar]
66.Farr A, Kiss H, Holzer I, Husslein P, Hagmann M, Petricevic L. Effect of asymptomatic vaginal colonization with Candida albicans on pregnancy outcome. Acta Obstet Gynecol Scand. 2015;94:989–96. doi: 10.1111/aogs.12697. [DOI] [PubMed] [Google Scholar]
67.Ward TL, Dominguez-Bello MG, Heisel T, Al-Ghalith G, Knights D, Gale CA. Development of the human mycobiome over the first month of life and across body sites. mSystems. 2018;3:e00140-17. doi: 10.1128/mSystems.00140-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
68.Bliss JM, Basavegowda KP, Watson WJ, Sheikh AU, Ryan RM. Vertical and horizontal transmission of Candida albicans in very low birth weight infants using DNA fingerprinting techniques. Pediatr Infect Dis J. 2008;27:231–5. doi: 10.1097/INF.0b013e31815bb69d. [DOI] [PubMed] [Google Scholar]
69.Brown SE, Schwartz JA, Robinson CK, O’Hanlon DE, Bradford LL, He X, et al. The vaginal microbiota and behavioral factors associated with genital Candida albicans detection in reproductive-age women. Sex Transm Dis. 2019;46:753–8. doi: 10.1097/OLQ.0000000000001066. [DOI] [PMC free article] [PubMed] [Google Scholar]
70.Guzel AB, Ilkit M, Akar T, Burgut R, Demir SC. Evaluation of risk factors in patients with vulvovaginal candidiasis and the value of chromID Candida agar versus CHROMagar Candida for recovery and presumptive identification of vaginal yeast species. Med Mycol. 2011;49:16–25. doi: 10.3109/13693786.2010.497972. [DOI] [PubMed] [Google Scholar]
71.Gonçalves B, Ferreira C, Alves CT, Henriques M, Azeredo J, Silva S. Vulvovaginal candidiasis: epidemiology, microbiology and risk factors. Crit Rev Microbiol. 2016;42:905–27. doi: 10.3109/1040841X.2015.1091805. [DOI] [PubMed] [Google Scholar]
72.Sobel JD. Vulvovaginal candidosis. Lancet. 2007;369::1961–71. doi: 10.1016/S0140-6736(07)60917-9. [DOI] [PubMed] [Google Scholar]
73.Fidel PL, Vazquez JA, Sobel JD. Candida glabrata: review of epidemiology, pathogenesis, and clinical disease with comparison to C. albicans. Clin Microbiol Rev. 1999;12:80–96. doi: 10.1128/CMR.12.1.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
74.Denning DW, Kneale M, Sobel JD, Rautemaa-Richardson R. Global burden of recurrent vulvovaginal candidiasis: a systematic review. Lancet Infect Dis. 2018;18:e339-47. doi: 10.1016/S1473-3099(18)30103-8. [DOI] [PubMed] [Google Scholar]
75.Förster TM, Mogavero S, Dräger A, Graf K, Polke M, Jacobsen ID, et al. Enemies and brothers in arms: Candida albicans and gram-positive bacteria. Cell Microbiol. 2016;18:1709–15. doi: 10.1111/cmi.12657. [DOI] [PubMed] [Google Scholar]
76.Sadeghi G, Ebrahimi-Rad M, Mousavi SF, Shams-Ghahfarokhi M, Razzaghi-Abyaneh M. Emergence of non-Candida albicans species: epidemiology, phylogeny and fluconazole susceptibility profile. J Mycol Med. 2018;28:51–8. doi: 10.1016/j.mycmed.2017.12.008. [DOI] [PubMed] [Google Scholar]
77.Ng KP, Kuan CS, Kaur H, Na SL, Atiya N, Velayuthan RD. Candida species epidemiology 2000–2013: a laboratory-based report. Trop Med Int Health. 2015;20:1447–53. doi: 10.1111/tmi.12577. [DOI] [PubMed] [Google Scholar]
78.Bitew A, Abebaw Y. Vulvovaginal candidiasis: species distribution of Candida and their antifungal susceptibility pattern. BMC Womens Health. 2018;18:94. doi: 10.1186/s12905-018-0607-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
79.De Vos MM, Cuenca-Estrella M, Boekhout T, Theelen B, Matthijs N, Bauters T, et al. Vulvovaginal candidiasis in a Flemish patient population. Clin Microbiol Infect. 2005;11:1005–11. doi: 10.1111/j.1469-0691.2005.01281.x. [DOI] [PubMed] [Google Scholar]
80.Rodríguez-Cerdeira C, Gregorio MC, Molares-Vila A, López-Barcenas A, Fabbrocini G, Bardhi B, et al. Biofilms and vulvovaginal candidiasis. Colloids Surf B Biointerfaces. 2019;174:110–25. doi: 10.1016/j.colsurfb.2018.11.011. [DOI] [PubMed] [Google Scholar]
81.Aballéa S, Guelfucci F, Wagner J, Khemiri A, Dietz J-P, Sobel J, et al. Subjective health status and health-related quality of life among women with recurrent vulvovaginal candidosis (RVVC) in Europe and the USA. Health Qual Life Outcomes. 2013;11:169. doi: 10.1186/1477-7525-11-169. [DOI] [PMC free article] [PubMed] [Google Scholar]
82.Nobile CJ, Johnson AD. Candida albicans biofilms and human disease. Annu Rev Microbiol. 2015;69:71–92. doi: 10.1146/annurev-micro-091014-104330. [DOI] [PMC free article] [PubMed] [Google Scholar]
83.Berman J. Candida albicans. Curr Biol. 2012;22:R620-2. doi: 10.1016/j.cub.2012.05.043. [DOI] [PubMed] [Google Scholar]
84.Bradford LL, Ravel J. The vaginal mycobiome: a contemporary perspective on fungi in women’s health and diseases. Virulence. 2017;8:342–51. doi: 10.1080/21505594.2016.1237332. [DOI] [PMC free article] [PubMed] [Google Scholar]
85.Swidsinski A, Guschin A, Tang Q, Dörffel Y, Verstraelen H, Tertychnyy A, et al. Vulvovaginal candidiasis: histologic lesions are primarily polymicrobial and invasive and do not contain biofilms. Am J Obstet Gynecol. 2019;220::91.e91-8. doi: 10.1016/j.ajog.2018.10.023. [DOI] [PubMed] [Google Scholar]
86.Roselletti E, Monari C, Sabbatini S, Perito S, Vecchiarelli A, Sobel JD, et al. A role for yeast/pseudohyphal cells of Candida albicans in the correlated expression of NLRP3 inflammasome inducers in women with acute vulvovaginal candidiasis. Front Microbiol. 2019;10:2669. doi: 10.3389/fmicb.2019.02669. [DOI] [PMC free article] [PubMed] [Google Scholar]
87.Krüger W, Vielreicher S, Kapitan M, Jacobsen ID, Niemiec MJ. Fungal-bacterial interactions in health and disease. Pathogens. 2019;8:70. doi: 10.3390/pathogens8020070. [DOI] [PMC free article] [PubMed] [Google Scholar]
88.Guo R, Zheng N, Lu H, Yin H, Yao J, Chen Y. Increased diversity of fungal flora in the vagina of patients with recurrent vaginal candidiasis and allergic rhinitis. Microb Ecol. 2012;64:918–27. doi: 10.1007/s00248-012-0084-0. [DOI] [PubMed] [Google Scholar]
89.Zheng N-N, Guo X-C, Lv W, Chen X-X, Feng G-F. Characterization of the vaginal fungal flora in pregnant diabetic women by 18S rRNA sequencing. Eur J Clin Microbiol Infect Dis. 2013;32:1031–40. doi: 10.1007/s10096-013-1847-3. [DOI] [PubMed] [Google Scholar]
90.Bradshaw CS, Brotman RM. Making inroads into improving treatment of bacterial vaginosis – striving for long-term cure. BMC Infect Dis. 2015;15:292. doi: 10.1186/s12879-015-1027-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
91.Peebles K, Velloza J, Balkus JE, McClelland RS, Barnabas RV. High global burden and costs of bacterial vaginosis: a systematic review and meta-Analysis. Sex Transm Dis. 2019;46:304–11. doi: 10.1097/OLQ.0000000000000972. [DOI] [PubMed] [Google Scholar]
92.Coleman JS, Gaydos CA. Molecular diagnosis of bacterial vaginosis: an update. J Clin Microbiol. 2018;56:e00342-18. doi: 10.1128/JCM.00342-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
93.Muzny CA, Laniewski P, Schwebke JR, Herbst-Kralovetz MM. Host–vaginal microbiota interactions in the pathogenesis of bacterial vaginosis. Curr Opin Infect Dis. 2020;33:59–65. doi: 10.1097/QCO.0000000000000620. [DOI] [PMC free article] [PubMed] [Google Scholar]
94.Ravel J, Brotman RM, Gajer P, Ma B, Nandy M, Fadrosh DW, et al. Daily temporal dynamics of vaginal microbiota before, during and after episodes of bacterial vaginosis. Microbiome. 2013;1::29. doi: 10.1186/2049-2618-1-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
95.Shimaoka M, Yo Y, Doh K, Kotani Y, Suzuki A, Tsuji I, et al. Association between preterm delivery and bacterial vaginosis with or without treatment. Sci Rep. 2019;9:509. doi: 10.1038/s41598-018-36964-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
96.Gondwe T, Ness R, Totten PA, Astete S, Tang G, Gold MA, et al. Novel bacterial vaginosis-associated organisms mediate the relationship between vaginal douching and pelvic inflammatory disease. Sex Transm Infect. 2020;96:439–44. doi: 10.1136/sextrans-2019-054191. [DOI] [PMC free article] [PubMed] [Google Scholar]
97.Bayigga L, Kateete DP, Anderson DJ, Sekikubo M, Nakanjako D. Diversity of vaginal microbiota in sub-Saharan Africa and its effects on HIV transmission and prevention. Am J Obstet Gynecol. 2019;220:155–66. doi: 10.1016/j.ajog.2018.10.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
98.Bilardi JE, Walker S, Temple-Smith M, McNair R, Mooney-Somers J, Bellhouse C, et al. The burden of bacterial vaginosis: women’s experience of the physical, emotional, sexual and social impact of living with recurrent bacterial vaginosis. PLoS One. 2013;8:e74378. doi: 10.1371/journal.pone.0074378. [DOI] [PMC free article] [PubMed] [Google Scholar]
99.Soper DE. Bacterial vaginosis and surgical site infections. Am J Obstet Gynecol. 2019;222:219–23. doi: 10.1016/j.ajog.2019.09.002. [DOI] [PubMed] [Google Scholar]
100.Muzny CA, Taylor CM, Swords WE, Tamhane A, Chattopadhyay D, Cerca N, et al. An updated conceptual model on the pathogenesis of bacterial vaginosis. J Infect Dis. 2019;220:1399–405. doi: 10.1093/infdis/jiz342. [DOI] [PMC free article] [PubMed] [Google Scholar]
101.Muzny CA, Blanchard E, Taylor CM, Aaron KJ, Talluri R, Griswold ME, et al. Identification of key bacteria involved in the induction of incident bacterial vaginosis: a prospective study. J Infect Dis. 2018;218:966–78. doi: 10.1093/infdis/jiy243. [DOI] [PMC free article] [PubMed] [Google Scholar]
102.Gilbert NM, Lewis WG, Li G, Sojka DK, Lubin JB, Lewis AL. Gardnerella vaginalis and Prevotella bivia trigger distinct and overlapping phenotypes in a mouse model of bacterial vaginosis. J Infect Dis. 2019;220:1099–108. doi: 10.1093/infdis/jiy704. [DOI] [PMC free article] [PubMed] [Google Scholar]
103.Castro J, Machado D, Cerca N. Unveiling the role of Gardnerella vaginalis in polymicrobial bacterial vaginosis biofilms: the impact of other vaginal pathogens living as neighbors. ISME J. 2019;13:1306–17. doi: 10.1038/s41396-018-0337-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
104.Swidsinski A, Mendling W, Loening-Baucke V, Swidsinski S, Dörffel Y, Scholze J, et al. An adherent Gardnerella vaginalis biofilm persists on the vaginal epithelium after standard therapy with oral metronidazole. Am J Obstet Gynecol. 2008;198::97.e91-6. doi: 10.1016/j.ajog.2007.06.039. [DOI] [PubMed] [Google Scholar]
105.Machado A, Cerca N. Influence of biofilm formation by Gardnerella vaginalis and other anaerobes on bacterial vaginosis. J Infect Dis. 2015;212:1856–61. doi: 10.1093/infdis/jiv338. [DOI] [PubMed] [Google Scholar]
106.Gosmann C, Anahtar MN, Handley SA, Farcasanu M, Abu-Ali G, Bowman BA, et al. Lactobacillus-deficient cervicovaginal bacterial communities are associated with increased HIV acquisition in young South African women. Immunity. 2017;46:29–37. doi: 10.1016/j.immuni.2016.12.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
107.Peipert JF, Lapane KL, Allsworth JE, Redding CA, Blume JD, Stein MD. Bacterial vaginosis, race, and sexually transmitted infections: does race modify the association? Sex Transm Dis. 2008;35:363–7. doi: 10.1097/OLQ.0b013e31815e4179. [DOI] [PubMed] [Google Scholar]
108.McClelland RS, Lingappa JR, Srinivasan S, Kinuthia J, John-Stewart GC, Jaoko W, et al. Evaluation of the association between the concentrations of key vaginal bacteria and the increased risk of HIV acquisition in African women from five cohorts: a nested case-control study. Lancet Infect Dis. 2018;18:554–64. doi: 10.1016/S1473-3099(18)30058-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
109.Cone RA. Vaginal microbiota and sexually transmitted infections that may influence transmission of cell-associated HIV. J Infect Dis. 2014;210::616-21. doi: 10.1093/infdis/jiu459. [DOI] [PMC free article] [PubMed] [Google Scholar]
110.Nardini P, Ñahui Palomino RA, Parolin C, Laghi L, Foschi C, Cevenini R, et al. Lactobacillus crispatus inhibits the infectivity of Chlamydia trachomatis elementary bodies, in vitro study. Sci Rep. 2016;6:29024. doi: 10.1038/srep29024. [DOI] [PMC free article] [PubMed] [Google Scholar]
111.Gong Z, Luna Y, Yu P, Fan H. Lactobacilli inactivate Chlamydia trachomatis through lactic acid but not H2O2. PLoS ONE. 2014;9:e107758. doi: 10.1371/journal.pone.0107758. [DOI] [PMC free article] [PubMed] [Google Scholar]
112.Rowley J, Vander Hoorn S, Korenromp E, Low N, Unemo M, Abu-Raddad LJ, et al. Chlamydia, gonorrhoea, trichomoniasis and syphilis: global prevalence and incidence estimates, 2016. Bull World Health Organ. 2019;97:548-62P. doi: 10.2471/BLT.18.228486. [DOI] [PMC free article] [PubMed] [Google Scholar]
113.Harp DF, Chowdhury I. Trichomoniasis: evaluation to execution. Eur J Obstet Gynecol Reprod Biol. 2011;157:3–9. doi: 10.1016/j.ejogrb.2011.02.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
114.McCormack D, Koons K. Sexually transmitted infections. Emerg Med Clin N Am. 2019;37:725–38. doi: 10.1016/j.emc.2019.07.009. [DOI] [PubMed] [Google Scholar]
115.Eisinger RW, Erbelding E, Fauci AS. Refocusing research on sexually transmitted infections. J Infect Dis. 2020;222:1432–1434. doi: 10.1093/infdis/jiz442. [DOI] [PMC free article] [PubMed] [Google Scholar]
116.Zhu H, Shen Z, Luo H, Zhang W, Zhu X. Chlamydia trachomatis infection-associated risk of cervical cancer: a meta-analysis. Med (Baltim) 2016;95:e3077. doi: 10.1097/MD.0000000000003077. [DOI] [PMC free article] [PubMed] [Google Scholar]
117.Johnson HL, Ghanem KG, Zenilman JM, Erbelding EJ. Sexually transmitted infections and adverse pregnancy outcomes among women attending inner city public sexually transmitted diseases clinics. Sex Transm Dis. 2011;38:167–71. doi: 10.1097/OLQ.0b013e3181f2e85f. [DOI] [PubMed] [Google Scholar]
118.van de Wijgert JHHM, Morrison CS, Brown J, Kwok C, Van Der Pol B, Chipato T, et al. Disentangling contributions of reproductive tract infections to HIV acquisition in African women. Sex Transm Dis. 2009;36:357–64. doi: 10.1097/OLQ.0b013e3181a4f695. [DOI] [PubMed] [Google Scholar]
119.Masson L, Barnabas S, Deese J, Lennard K, Dabee S, Gamieldien H, et al. Inflammatory cytokine biomarkers of asymptomatic sexually transmitted infections and vaginal dysbiosis: a multicentre validation study. Sex Transm Infect. 2019;95:5–12. doi: 10.1136/sextrans-2017-053506. [DOI] [PubMed] [Google Scholar]
120.Brotman RM, Bradford LL, Conrad M, Gajer P, Ault K, Peralta L, et al. Association between Trichomonas vaginalis and vaginal bacterial community composition among reproductive-age women. Sex Transm Dis. 2012;39:807–12. doi: 10.1097/OLQ.0b013e3182631c79. [DOI] [PMC free article] [PubMed] [Google Scholar]
121.Galvin SR, Cohen MS. The role of sexually transmitted diseases in HIV transmission. Nat Rev Microbiol. 2004;2:33–42. doi: 10.1038/nrmicro794. [DOI] [PubMed] [Google Scholar]
122.Lewis J, Price MJ, Horner PJ, White PJ. Genital Chlamydia trachomatis infections clear more slowly in men than women, but are less likely to become established. J Infect Dis. 2017;216:237–44. doi: 10.1093/infdis/jix283. [DOI] [PMC free article] [PubMed] [Google Scholar]
123.Stapleton AE. The vaginal microbiota and urinary tract infection. Microbiol Spectrom. 2016 doi: 10.1128/microbiolspec.UTI-0025-2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
124.Qiao L-D, Chen S, Yang Y, Zhang K, Zheng B, Guo H-F, et al. Characteristics of urinary tract infection pathogens and their in vitro susceptibility to antimicrobial agents in China: data from a multicenter study. BMJ Open. 2013;3:e004152. doi: 10.1136/bmjopen-2013-004152. [DOI] [PMC free article] [PubMed] [Google Scholar]
125.Flores-Mireles AL, Walker JN, Caparon M, Hultgren SJ. Urinary tract infections: epidemiology, mechanisms of infection and treatment options. Nat Rev Microbiol. 2015;13:269–84. doi: 10.1038/nrmicro3432. [DOI] [PMC free article] [PubMed] [Google Scholar]
126.Kline KA, Lewis AL. Gram-positive uropathogens, polymicrobial urinary tract infection, and the emerging microbiota of the urinary tract. Microbiol Spectr. 2016 doi: 10.1128/microbiolspec.UTI-0012-2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
127.Kwon YE, Oh D-J, Kim MJ, Choi HM. Prevalence and clinical characteristics of asymptomatic pyuria in chronic kidney disease. Ann Lab Med. 2020;40:238–44. doi: 10.3343/alm.2020.40.3.238. [DOI] [PMC free article] [PubMed] [Google Scholar]
128.Chu CM, Lowder JL. Diagnosis and treatment of urinary tract infections across age groups. Am J Obstet Gynecol. 2018;219:40–51. doi: 10.1016/j.ajog.2017.12.231. [DOI] [PubMed] [Google Scholar]
129.Thomas-White K, Forster SC, Kumar N, Van Kuiken M, Putonti C, Stares MD, et al. Culturing of female bladder bacteria reveals an interconnected urogenital microbiota. Nat Commun. 2018;9:1557. doi: 10.1038/s41467-018-03968-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
130.Terlizzi ME, Gribaudo G, Maffei ME. UroPathogenic Escherichia coli (UPEC) infections: virulence factors, bladder responses, antibiotic, and non-antibiotic antimicrobial strategies. Front Microbiol. 2017;8:1566. doi: 10.3389/fmicb.2017.01566. [DOI] [PMC free article] [PubMed] [Google Scholar]
131.Komesu YM, Dinwiddie DL, Richter HE, Lukacz ES, Sung VW, Siddiqui NY, et al. Defining the relationship between vaginal and urinary microbiomes. Am J Obstet Gynecol. 2020;222:151.e1-10. doi: 10.1016/j.ajog.2019.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
132.Kirjavainen PV, Pautler S, Baroja ML, Anukam K, Crowley K, Carter K, et al. Abnormal immunological profile and vaginal microbiota in women prone to urinary tract infections. Clin Vaccine Immunol. 2009;16:29–36. doi: 10.1128/CVI.00323-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
133.Gilbert NM, O’Brien VP, Lewis AL. Transient microbiota exposures activate dormant Escherichia coli infection in the bladder and drive severe outcomes of recurrent disease. PLoS Pathog. 2017;13:e1006238. doi: 10.1371/journal.ppat.1006238. [DOI] [PMC free article] [PubMed] [Google Scholar]
134.Pierson JD, Hansmann MA, Davis CC, Forney LJ. The effect of vaginal microbial communities on colonization by Staphylococcus aureus with the gene for toxic shock syndrome toxin 1 (TSST-1): a case–control study. Pathog Dis. 2018;76:fty015. doi: 10.1093/femspd/fty015. [DOI] [PMC free article] [PubMed] [Google Scholar]
135.Schlievert PM, Nemeth KA, Davis CC, Peterson ML, Jones BE. Staphylococcus aureus exotoxins are present in vivo in tampons. Clin Vaccine Immunol. 2010;17:722–7. doi: 10.1128/CVI.00483-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
136.Schlievert PM. Effect of non-absorbent intravaginal menstrual/contraceptive products on Staphylococcus aureus and production of the superantigen TSST-1. Eur J Clin Microbiol Infect Dis. 2020;39:31–8. doi: 10.1007/s10096-019-03685-x. [DOI] [PubMed] [Google Scholar]
137.Nonfoux L, Chiaruzzi M, Badiou C, Baude J, Tristan A, Thioulouse J, et al. Impact of currently marketed tampons and menstrual cups on Staphylococcus aureus growth and toxic shock syndrome toxin 1 production in vitro. Appl Environ Microbiol. 2018;84:e00351-18. doi: 10.1128/AEM.00351-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
138.Carter K, Bassis C, McKee K, Bullock K, Eastman A, Young V, et al. The impact of tampon use on the vaginal microbiota across four menstrual cycles. Am J Obstet Gynecol. 2018;219:639. doi: 10.1016/j.ajog.2018.10.078. [DOI] [Google Scholar]
139.MacPhee RA, Miller WL, Gloor GB, McCormick JK, Hammond J-A, Burton JP, et al. Influence of the vaginal microbiota on toxic shock syndrome toxin 1 production by Staphylococcus aureus. Appl Environ Microbiol. 2013;79:1835–42. doi: 10.1128/AEM.02908-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
140.Leroy F, De Vuyst L. Lactic acid bacteria as functional starter cultures for the food fermentation industry. Trends Food Sci Technol. 2004;15:67–78. doi: 10.1016/j.tifs.2003.09.004. [DOI] [Google Scholar]
141.George F, Daniel C, Thomas M, Singer E, Guilbaud A, Tessier FJ, et al. Occurrence and dynamism of lactic acid bacteria in distinct ecological niches: a multifaceted functional health perspective. Front Microbiol. 2018;9:2899. doi: 10.3389/fmicb.2018.02899. [DOI] [PMC free article] [PubMed] [Google Scholar]
142.Kerry RG, Patra JK, Gouda S, Park Y, Shin H-S, Das G. Benefaction of probiotics for human health: a review. J Food Drug Anal. 2018;26:927–39. doi: 10.1016/j.jfda.2018.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
143.Ghosh T, Beniwal A, Semwal A, Navani NK. Mechanistic insights into probiotic properties of lactic acid bacteria associated with ethnic fermented dairy products. Front Microbiol. 2019;10:502. doi: 10.3389/fmicb.2019.00502. [DOI] [PMC free article] [PubMed] [Google Scholar]
144.Mattia A, Merker R. Regulation of probiotic substances as ingredients in foods: premarket approval or “Generally Recognized as Safe” notification. Clin Infect Dis. 2008;46::115-8. doi: 10.1086/523329. [DOI] [PubMed] [Google Scholar]
145.Venegas-Ortega MG, Flores-Gallegos AC, Martínez-Hernández JL, Aguilar CN, Nevárez-Moorillón GV. Production of bioactive peptides from lactic acid bacteria: a sustainable approach for healthier foods. Compr Rev Food Sci Food Saf. 2019;18:1039–51. doi: 10.1111/1541-4337.12455. [DOI] [PubMed] [Google Scholar]
146.Iyer R, Tomar SK, Uma Maheswari T, Singh R. Streptococcus thermophilus strains: multifunctional lactic acid bacteria. Int Dairy J. 2010;20:133–41. doi: 10.1016/j.idairyj.2009.10.005. [DOI] [Google Scholar]
147.Cui Y, Xu T, Qu X, Hu T, Jiang X, Zhao C. New insights into various production characteristics of Streptococcus thermophilus strains. Int J Mol Sci. 2016;17:1701. doi: 10.3390/ijms17101701. [DOI] [PMC free article] [PubMed] [Google Scholar]
148.Reid G, Younes JA, Van der Mei HC, Gloor GB, Knight R, Busscher HJ. Microbiota restoration: natural and supplemented recovery of human microbial communities. Nat Rev Microbiol. 2010;9:27. doi: 10.1038/nrmicro2473. [DOI] [PubMed] [Google Scholar]
149.Prabhurajeshwar C, Chandrakanth RK. Probiotic potential of lactobacilli with antagonistic activity against pathogenic strains: an in vitro validation for the production of inhibitory substances. Biomed J. 2017;40:270–83. doi: 10.1016/j.bj.2017.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
150.Chew SY, Cheah YK, Seow HF, Sandai D, Than LTL. Probiotic Lactobacillus rhamnosus GR-1 and Lactobacillus reuteri RC-14 exhibit strong antifungal effects against vulvovaginal candidiasis-causing Candida glabrata isolates. J Appl Microbiol. 2015;118:1180–90. doi: 10.1111/jam.12772. [DOI] [PMC free article] [PubMed] [Google Scholar]
151.Singh TP, Kaur G, Kapila S, Malik RK. Antagonistic activity of Lactobacillus reuteri strains on the adhesion characteristics of selected pathogens. Front Microbiol. 2017;8:486. doi: 10.3389/fmicb.2017.00486. [DOI] [PMC free article] [PubMed] [Google Scholar]
152.Humphreys GJ, McBain AJ. Antagonistic effects of Streptococcus and Lactobacillus probiotics in pharyngeal biofilms. Lett Appl Microbiol. 2019;68:303–12. doi: 10.1111/lam.13133. [DOI] [PubMed] [Google Scholar]
153.Gaspar C, Donders GG, Palmeira-de-Oliveira R, Queiroz JA, Tomaz C, Martinez-de-Oliveira J, et al. Bacteriocin production of the probiotic Lactobacillus acidophilus KS400. AMB Express. 2018;8:153. doi: 10.1186/s13568-018-0679-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
154.Turovskiy Y, Ludescher RD, Aroutcheva AA, Faro S, Chikindas ML. Lactocin 160, a bacteriocin produced by vaginal Lactobacillus rhamnosus, targets cytoplasmic membranes of the vaginal pathogen, Gardnerella vaginalis. Probiotics Antimicrob Proteins. 2009;1:67–74. doi: 10.1007/s12602-008-9003-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
155.Donders GGG, Ruban K, Bellen G. Selecting anti-microbial treatment of aerobic vaginitis. Curr Infect Dis Rep. 2015;17:477. doi: 10.1007/s11908-015-0477-6. [DOI] [PubMed] [Google Scholar]
156.Donders GGG, Bellen G, Grinceviciene S, Ruban K, Vieira-Baptista P. Aerobic vaginitis: no longer a stranger. Res Microbiol. 2017;168:845–58. doi: 10.1016/j.resmic.2017.04.004. [DOI] [PubMed] [Google Scholar]
157.Beigi RH, Austin MN, Meyn LA, Krohn MA, Hillier SL. Antimicrobial resistance associated with the treatment of bacterial vaginosis. Am J Obstet Gynecol. 2004;191:1124–9. doi: 10.1016/j.ajog.2004.05.033. [DOI] [PubMed] [Google Scholar]
158.Austin MN, Beigi RH, Meyn LA, Hillier SL. Microbiologic response to treatment of bacterial vaginosis with topical clindamycin or metronidazole. J Clin Microbiol. 2005;43:4492–7. doi: 10.1128/JCM.43.9.4492-4497.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
159.Bertuccini L, Russo R, Iosi F, Superti F. Effects of Lactobacillus rhamnosus and Lactobacillus acidophilus on bacterial vaginal pathogens. Int J Immunopathol Pharmacol. 2017;30:163–7. doi: 10.1177/0394632017697987. [DOI] [PMC free article] [PubMed] [Google Scholar]
160.De Alberti D, Russo R, Terruzzi F, Nobile V, Ouwehand AC. Lactobacilli vaginal colonisation after oral consumption of Respecta® complex: a randomised controlled pilot study. Arch Gynecol Obstet. 2015;292:861–7. doi: 10.1007/s00404-015-3711-4. [DOI] [PubMed] [Google Scholar]
161.Mezzasalma V, Manfrini E, Ferri E, Boccarusso M, Di Gennaro P, Schiano I, et al. Orally administered multispecies probiotic formulations to prevent uro-genital infections: a randomized placebo-controlled pilot study. Arch Gynecol Obstet. 2017;295:163–72. doi: 10.1007/s00404-016-4235-2. [DOI] [PubMed] [Google Scholar]
162.Wang S, Wang Q, Yang E, Yan L, Li T, Zhuang H. Antimicrobial compounds produced by vaginal Lactobacillus crispatus are able to strongly inhibit Candida albicans growth, hyphal formation and regulate virulence-related gene expressions. Front Microbiol. 2017;8:564. doi: 10.3389/fmicb.2017.00564. [DOI] [PMC free article] [PubMed] [Google Scholar]
163.Li T, Liu Z, Zhang X, Chen X, Wang S. Local probiotic Lactobacillus crispatus and Lactobacillus delbrueckii exhibit strong antifungal effects against vulvovaginal candidiasis in a rat model. Front Microbiol. 2019;10:1033. doi: 10.3389/fmicb.2019.01033. [DOI] [PMC free article] [PubMed] [Google Scholar]
164.Heczko PB, Tomusiak A, Adamski P, Jakimiuk AJ, Stefański G, Mikołajczyk-Cichońska A, et al. Supplementation of standard antibiotic therapy with oral probiotics for bacterial vaginosis and aerobic vaginitis: a randomised, double-blind, placebo-controlled trial. BMC Womens Health. 2015;15:115. doi: 10.1186/s12905-015-0246-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
165.Balzaretti S, Taverniti V, Rondini G, Marcolegio G, Minuzzo M, Remagni MC, et al. The vaginal isolate Lactobacillus paracasei LPC-S01 (DSM 26760) is suitable for oral administration. Front Microbiol. 2015;6:952. doi: 10.3389/fmicb.2015.00952. [DOI] [PMC free article] [PubMed] [Google Scholar]
166.Reid G, Bruce AW, Fraser N, Heinemann C, Owen J, Henning B. Oral probiotics can resolve urogenital infections. FEMS Immunol Med Microbiol. 2001;30:49–52. doi: 10.1111/j.1574-695X.2001.tb01549.x. [DOI] [PubMed] [Google Scholar]
167.Buggio L, Somigliana E, Borghi A, Vercellini P. Probiotics and vaginal microecology: fact or fancy? BMC Womens Health. 2019;19:25. doi: 10.1186/s12905-019-0723-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
168.Bohbot JM, Daraï E, Bretelle F, Brami G, Daniel C, Cardot JM. Efficacy and safety of vaginally administered lyophilized Lactobacillus crispatus IP 174178 in the prevention of bacterial vaginosis recurrence. J Gynecol Obstet Hum Reprod. 2018;47:81–6. doi: 10.1016/j.jogoh.2017.11.005. [DOI] [PubMed] [Google Scholar]
169.Vicariotto F, Mogna L, Del Piano M. Effectiveness of the two microorganisms Lactobacillus fermentum LF15 and Lactobacillus plantarum LP01, formulated in slow-release vaginal tablets, in women affected by bacterial vaginosis: a pilot study. J Clin Gastroenterol. 2014;48:106–112. doi: 10.1097/MCG.0000000000000226. [DOI] [PubMed] [Google Scholar]
170.Palma E, Recine N, Domenici L, Giorgini M, Pierangeli A, Panici PB. Long-term Lactobacillus rhamnosus BMX 54 application to restore a balanced vaginal ecosystem: a promising solution against HPV-infection. BMC Infect Dis. 2018;18:13. doi: 10.1186/s12879-017-2938-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
171.Recine N, Palma E, Domenici L, Giorgini M, Imperiale L, Sassu C, et al. Restoring vaginal microbiota: biological control of bacterial vaginosis. A prospective case–control study using Lactobacillus rhamnosus BMX 54 as adjuvant treatment against bacterial vaginosis. Arch Gynecol Obstet. 2016;293:101–7. doi: 10.1007/s00404-015-3810-2. [DOI] [PubMed] [Google Scholar]
172.van de Wijgert JHHM, Verwijs MC, Agaba SK, Bronowski C, Mwambarangwe L, Uwineza M, et al. Intermittent lactobacilli-containing vaginal probiotic or metronidazole use to prevent bacterial vaginosis recurrence: a pilot study incorporating microscopy and sequencing. Sci Rep. 2020;10:3884. doi: 10.1038/s41598-020-60671-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
173.Russo R, Superti F, Karadja E, De Seta F. Randomised clinical trial in women with recurrent vulvovaginal candidiasis: efficacy of probiotics and lactoferrin as maintenance treatment. Mycoses. 2019;62:328–35. doi: 10.1111/myc.12883. [DOI] [PubMed] [Google Scholar]
174.Xie HY, Feng D, Wei DM, Mei L, Chen H, Wang X, et al. Probiotics for vulvovaginal candidiasis in non-pregnant women. Cochrane Database Syst Rev. 2017;11:CD010496. doi: 10.1002/14651858.CD010496.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
175.Chehoud C, Stieh DJ, Bailey AG, Laughlin AL, Allen SA, McCotter KL, et al. Associations of the vaginal microbiota with HIV infection, bacterial vaginosis, and demographic factors. AIDS. 2017;31:895–904. doi: 10.1097/QAD.0000000000001421. [DOI] [PMC free article] [PubMed] [Google Scholar]
176.Spear GT, St John E, Zariffard M. Bacterial vaginosis and human immunodeficiency virus infection. AIDS Res Ther. 2007;4:25. doi: 10.1186/1742-6405-4-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
177.Brichacek B, Lagenaur LA, Lee PP, Venzon D, Hamer DH. In vivo evaluation of safety and toxicity of a Lactobacillus jensenii producing modified cyanovirin-N in a rhesus macaque vaginal challenge model. PLoS One. 2013;8:e78817. doi: 10.1371/journal.pone.0078817. [DOI] [PMC free article] [PubMed] [Google Scholar]
178.Palomino RAN, Zicari S, Vanpouille C, Vitali B, Margolis L. Vaginal Lactobacillus inhibits HIV-1 replication in human tissues ex vivo. Front Microbiol. 2017;8:906. doi: 10.3389/fmicb.2017.00906. [DOI] [PMC free article] [PubMed] [Google Scholar]
179.Martín V, Maldonado A, Fernández L, Rodríguez JM, Connor RI. Inhibition of human immunodeficiency virus type 1 by lactic acid bacteria from human breastmilk. Breastfeed Med. 2010;5:153–8. doi: 10.1089/bfm.2010.0001. [DOI] [PMC free article] [PubMed] [Google Scholar]
180.Su Y, Zhang B, Su L. CD4 detected from Lactobacillus helps understand the interaction between Lactobacillus and HIV. Microbiol Res. 2013;168:273–7. doi: 10.1016/j.micres.2012.12.004. [DOI] [PubMed] [Google Scholar]
181.Palomino RAÑ, Vanpouille C, Laghi L, Parolin C, Melikov K, Backlund P, et al. Extracellular vesicles from symbiotic vaginal lactobacilli inhibit HIV-1 infection of human tissues. Nat Commun. 2019;10:5656. doi: 10.1038/s41467-019-13468-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
182.Spurbeck RR, Arvidson CG. Lactobacilli at the front line of defense against vaginally acquired infections. Future Microbiol. 2011;6:567–82. doi: 10.2217/fmb.11.36. [DOI] [PubMed] [Google Scholar]
183.Sanders ME, Merenstein DJ, Reid G, Gibson GR, Rastall RA. Probiotics and prebiotics in intestinal health and disease: from biology to the clinic. Nat Rev Gastroenterol Hepatol. 2019;16:605–16. doi: 10.1038/s41575-019-0173-3. [DOI] [PubMed] [Google Scholar]
184.Lebeer S, Vanderleyden J, De Keersmaecker SCJ. Genes and molecules of lactobacilli supporting probiotic action. Microbiol Mol Biol Rev. 2008;72:728–64. doi: 10.1128/MMBR.00017-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
185.Lebeer S, Vanderleyden J, De Keersmaecker SC. Host interactions of probiotic bacterial surface molecules: comparison with commensals and pathogens. Nat Rev Microbiol. 2010;8:171–84. doi: 10.1038/nrmicro2297. [DOI] [PubMed] [Google Scholar]
186.Hajfarajollah H, Eslami P, Mokhtarani B, Akbari Noghabi K. Biosurfactants from probiotic bacteria: a review. Biotechnol Appl Biochem. 2018;65:768–83. doi: 10.1002/bab.1686. [DOI] [PubMed] [Google Scholar]
187.Sanders ME, Benson A, Lebeer S, Merenstein DJ, Klaenhammer TR. Shared mechanisms among probiotic taxa: implications for general probiotic claims. Curr Opin Biotechnol. 2018;49:207–16. doi: 10.1016/j.copbio.2017.09.007. [DOI] [PubMed] [Google Scholar]
188.Duchêne M-C, Rolain T, Knoops A, Courtin P, Chapot-Chartier M-P, Dufrêne YF, et al. Distinct and specific role of NlpC/P60 endopeptidases LytA and LytB in cell elongation and division of Lactobacillus plantarum. Front Microbiol. 2019;10:713. doi: 10.3389/fmicb.2019.00713. [DOI] [PMC free article] [PubMed] [Google Scholar]
189.Delcour J, Ferain T, Deghorain M, Palumbo E, Hols P. The biosynthesis and functionality of the cell-wall of lactic acid bacteria. Antonie Van Leeuwenhoek. 1999;76:159–84. doi: 10.1023/A:1002089722581. [DOI] [PubMed] [Google Scholar]
190.Chapot-Chartier M-P, Kulakauskas S. Cell wall structure and function in lactic acid bacteria. Microb Cell Fact. 2014;13:9. doi: 10.1186/1475-2859-13-S1-S9. [DOI] [PMC free article] [PubMed] [Google Scholar]
191.Liu Y, Perez J, Hammer LA, Gallagher HC, De Jesus M, Egilmez NK, et al. Intravaginal administration of interleukin 12 during genital gonococcal infection in mice induces immunity to heterologous strains of Neisseria gonorrhoeae. mSphere. 2018;3:e00421-17. doi: 10.1128/mSphere.00421-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
192.Shida K, Kiyoshima-Shibata J, Kaji R, Nagaoka M, Nanno M. Peptidoglycan from lactobacilli inhibits interleukin-12 production by macrophages induced by Lactobacillus casei through Toll-like receptor 2-dependent and independent mechanisms. Immunology. 2009;128:e858-69. doi: 10.1111/j.1365-2567.2009.03095.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
193.Choi S-H, Lee S-H, Kim MG, Lee HJ, Kim G-B. Lactobacillus plantarum CAU1055 ameliorates inflammation in lipopolysaccharide-induced RAW264.7 cells and a dextran sulfate sodium–induced colitis animal model. J Dairy Sci. 2019;102:6718–25. doi: 10.3168/jds.2018-16197. [DOI] [PubMed] [Google Scholar]
194.Wu Z, Pan D-d, Guo Y, Zeng X. Structure and anti-inflammatory capacity of peptidoglycan from Lactobacillus acidophilus in RAW-264.7 cells. Carbohydr Polym. 2013;96:466–73. doi: 10.1016/j.carbpol.2013.04.028. [DOI] [PubMed] [Google Scholar]
195.Song J, Lang F, Zhao N, Guo Y, Zhang H. Vaginal lactobacilli induce differentiation of monocytic precursors toward Langerhans-like cells: in vitro evidence. Front Immunol. 2018;9:2437. doi: 10.3389/fimmu.2018.02437. [DOI] [PMC free article] [PubMed] [Google Scholar]
196.Torcia MG. Interplay among vaginal microbiome, immune response and sexually transmitted viral infections. Int J Mol Sci. 2019;20:266. doi: 10.3390/ijms20020266. [DOI] [PMC free article] [PubMed] [Google Scholar]
197.Mastromarino P, Cacciotti F, Masci A, Mosca L. Antiviral activity of Lactobacillus brevis towards herpes simplex virus type 2: role of cell wall associated components. Anaerobe. 2011;17:334–6. doi: 10.1016/j.anaerobe.2011.04.022. [DOI] [PubMed] [Google Scholar]
198.Bron PA, Tomita S, van Swam II, Remus DM, Meijerink M, Wels M, et al. Lactobacillus plantarum possesses the capability for wall teichoic acid backbone alditol switching. Microb Cell Fact. 2012;11:123. doi: 10.1186/1475-2859-11-123. [DOI] [PMC free article] [PubMed] [Google Scholar]
199.Andre G, Deghorain M, Bron PA, van Swam II, Kleerebezem M, Hols P, et al. Fluorescence and atomic force microscopy imaging of wall teichoic acids in Lactobacillus plantarum. ACS Chem Biol. 2011;6:366–76. doi: 10.1021/cb1003509. [DOI] [PubMed] [Google Scholar]
200.Tomita S, Irisawa T, Tanaka N, Nukada T, Satoh E, Uchimura T, et al. Comparison of components and synthesis genes of cell wall teichoic acid among Lactobacillus plantarum strains. Biosci Biotechnol Biochem. 2010;74:928–33. doi: 10.1271/bbb.90736. [DOI] [PubMed] [Google Scholar]
201.Hardy L, Cerca N, Jespers V, Vaneechoutte M, Crucitti T. Bacterial biofilms in the vagina. Res Microbiol. 2017;168:865–74. doi: 10.1016/j.resmic.2017.02.001. [DOI] [PubMed] [Google Scholar]
202.Jung S, Park O-J, Kim AR, Ahn KB, Lee D, Kum K-Y, et al. Lipoteichoic acids of lactobacilli inhibit Enterococcus faecalis biofilm formation and disrupt the preformed biofilm. J Microbiol. 2019;57::310–15. doi: 10.1007/s12275-019-8538-4. [DOI] [PubMed] [Google Scholar]
203.Kim AR, Ahn KB, Yun C-H, Park O-J, Perinpanayagam H, Yoo Y-J, et al. Lactobacillus plantarum lipoteichoic acid inhibits oral multispecies biofilm. J Endod. 2019;45:310–5. doi: 10.1016/j.joen.2018.12.007. [DOI] [PubMed] [Google Scholar]
204.Vidal K, Donnet-Hughes A, Granato D. Lipoteichoic acids from Lactobacillus johnsonii strain La1 and Lactobacillus acidophilus strain La10 antagonize the responsiveness of human intestinal epithelial HT29 cells to lipopolysaccharide and gram-negative bacteria. Infect Immun. 2002;70::2057–64. doi: 10.1128/IAI.70.4.2057-2064.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
205.Ahn JE, Kim H, Chung DK. Lipoteichoic acid isolated from Lactobacillus plantarum maintains inflammatory homeostasis through regulation of Th1- and Th2-induced cytokines. J Microbiol Biotechnol. 2019;29:151–9. doi: 10.4014/jmb.1809.09001. [DOI] [PubMed] [Google Scholar]
206.Pericolini E, Perito S, Castagnoli A, Gabrielli E, Mencacci A, Blasi E, et al. Epitope unmasking in vulvovaginal candidiasis is associated with hyphal growth and neutrophilic infiltration. PLoS One. 2018;13:e0201436. doi: 10.1371/journal.pone.0201436. [DOI] [PMC free article] [PubMed] [Google Scholar]
207.Hassan AN, Frank JF, Shalabi SI. Factors affecting capsule size and production by lactic acid bacteria used as dairy starter cultures. Int J Food Microbiol. 2001;64:199–203. doi: 10.1016/S0168-1605(00)00427-X. [DOI] [PubMed] [Google Scholar]
208.Poole J, Day CJ, von Itzstein M, Paton JC, Jennings MP. Glycointeractions in bacterial pathogenesis. Nat Rev Microbiol. 2018;16:440–52. doi: 10.1038/s41579-018-0007-2. [DOI] [PubMed] [Google Scholar]
209.Laiño J, Villena J, Kanmani P, Kitazawa H. Immunoregulatory effects triggered by lactic acid bacteria exopolysaccharides: new insights into molecular interactions with host cells. Microorganisms. 2016;4:27. doi: 10.3390/microorganisms4030027. [DOI] [PMC free article] [PubMed] [Google Scholar]
210.Badel S, Bernardi T, Michaud P. New perspectives for lactobacilli exopolysaccharides. Biotechnol Adv. 2011;29:54–66. doi: 10.1016/j.biotechadv.2010.08.011. [DOI] [PubMed] [Google Scholar]
211.Shukla A, Mehta K, Parmar J, Pandya J, Saraf M. Depicting the exemplary knowledge of microbial exopolysaccharides in a nutshell. Eur Polym J. 2019;119:298–310. doi: 10.1016/j.eurpolymj.2019.07.044. [DOI] [Google Scholar]
212.Salazar N, Gueimonde M, de los Reyes-Gavilán CG, Ruas-Madiedo P. Exopolysaccharides produced by lactic acid bacteria and bifidobacteria as fermentable substrates by the intestinal microbiota. Crit Rev Food Sci Nutr. 2016;56:1440–53. doi: 10.1080/10408398.2013.770728. [DOI] [PubMed] [Google Scholar]
213.Ruas-Madiedo P, Medrano M, Salazar N, De Los Reyes-Gavilán CG, Pérez PF, Abraham AG. Exopolysaccharides produced by Lactobacillus and Bifidobacterium strains abrogate in vitro the cytotoxic effect of bacterial toxins on eukaryotic cells. J Appl Microbiol. 2010;109::2079–86. doi: 10.1111/j.1365-2672.2010.04839.x. [DOI] [PubMed] [Google Scholar]
214.Gamar-Nourani L, Blondeau K, Simonet J-M. Influence of culture conditions on exopolysaccharide production by Lactobacillus rhamnosus strain C83. J Appl Microbiol. 1998;85:664–72. doi: 10.1111/j.1365-2672.1998.00574.x. [DOI] [Google Scholar]
215.Lin T, Chen C, Chen B, Shaw J, Chen Y. Optimal economic productivity of exopolysaccharides from lactic acid bacteria with production possibility curves. Food Sci Nutr. 2019;7:2336–44. doi: 10.1002/fsn3.1079. [DOI] [PMC free article] [PubMed] [Google Scholar]
216.Bertsch A, Roy D, LaPointe G. Enhanced exopolysaccharide production by Lactobacillus rhamnosus in co-culture with Saccharomyces cerevisiae. Appl Sci. 2019;9:4026. doi: 10.3390/app9194026. [DOI] [Google Scholar]
217.Sánchez J-I, Martínez B, Guillén R, Jiménez-Díaz R, Rodríguez A. Culture conditions determine the balance between two different exopolysaccharides produced by Lactobacillus pentosus LPS26. Appl Environ Microbiol. 2006;72:7495–502. doi: 10.1128/AEM.01078-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
218.Imran MYM, Reehana N, Jayaraj KA, Ahamed AAP, Dhanasekaran D, Thajuddin N, et al. Statistical optimization of exopolysaccharide production by Lactobacillus plantarum NTMI05 and NTMI20. Int J Biol Macromol. 2016;93:731–45. doi: 10.1016/j.ijbiomac.2016.09.007. [DOI] [PubMed] [Google Scholar]
219.Cheng X, Huang L, Li K-t. Antioxidant activity changes of exopolysaccharides with different carbon sources from Lactobacillus plantarum LPC-1 and its metabolomic analysis. World J Microbiol Biotechnol. 2019;35:68. doi: 10.1007/s11274-019-2645-6. [DOI] [PubMed] [Google Scholar]
220.Patten DA, Laws AP. Lactobacillus-produced exopolysaccharides and their potential health benefits: a review. Benef Microbes. 2015;6:457–71. doi: 10.3920/BM2014.0117. [DOI] [PubMed] [Google Scholar]
221.Rahbar Saadat Y, Yari Khosroushahi A, Pourghassem Gargari B. A comprehensive review of anticancer, immunomodulatory and health beneficial effects of the lactic acid bacteria exopolysaccharides. Carbohydr Polym. 2019;217:79–89. doi: 10.1016/j.carbpol.2019.04.025. [DOI] [PubMed] [Google Scholar]
222.El-Deeb NM, Yassin AM, Al-Madboly LA, El-Hawiet A. A novel purified Lactobacillus acidophilus 20079 exopolysaccharide, LA-EPS-20079, molecularly regulates both apoptotic and NF-κB inflammatory pathways in human colon cancer. Microb Cell Fact. 2018;17:29. doi: 10.1186/s12934-018-0877-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
223.Tukenmez U, Aktas B, Aslim B, Yavuz S. The relationship between the structural characteristics of lactobacilli-EPS and its ability to induce apoptosis in colon cancer cells in vitro. Sci Rep. 2019;9:8268. doi: 10.1038/s41598-019-44753-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
224.Allonsius CN, van den Broek MFL, De Boeck I, Kiekens S, Oerlemans EFM, Kiekens F, et al. Interplay between Lactobacillus rhamnosus GG and Candida and the involvement of exopolysaccharides. Microb Biotechnol. 2017;10:1753–63. doi: 10.1111/1751-7915.12799. [DOI] [PMC free article] [PubMed] [Google Scholar]
225.Meade KG, O’Farrelly C. β-defensins: Farming the microbiome for homeostasis and health. Front Immunol. 2019;9:3072. doi: 10.3389/fimmu.2018.03072. [DOI] [PMC free article] [PubMed] [Google Scholar]
226.Donnarumma G, Molinaro A, Cimini D, De Castro C, Valli V, De Gregorio V, et al. Lactobacillus crispatus L1: high cell density cultivation and exopolysaccharide structure characterization to highlight potentially beneficial effects against vaginal pathogens. BMC Microbiol. 2014;14:137. doi: 10.1186/1471-2180-14-137. [DOI] [PMC free article] [PubMed] [Google Scholar]
227.Sudbery PE. Growth of Candida albicans hyphae. Nat Rev Microbiol. 2011;9:737. doi: 10.1038/nrmicro2636. [DOI] [PubMed] [Google Scholar]
228.Machado D, Castro J, Palmeira-de-Oliveira A, Martinez-de-Oliveira J, Cerca N. Bacterial vaginosis biofilms: challenges to current therapies and emerging solutions. Front Microbiol. 2016;6:1528. doi: 10.3389/fmicb.2015.01528. [DOI] [PMC free article] [PubMed] [Google Scholar]
229.Chen Z, Zhang Z, Zhang H, Xie B. Analysis of the oxidative stress status in nonspecific vaginitis and its role in vaginal epithelial cells apoptosis. Biomed Res Int. 2015;2015:795656. doi: 10.1155/2015/795656. [DOI] [PMC free article] [PubMed] [Google Scholar]
230.Hoang T, Toler E, DeLong K, Mafunda NA, Bloom SM, Zierden HC, et al. The cervicovaginal mucus barrier to HIV-1 is diminished in bacterial vaginosis. PLoS Pathog. 2020;16:e1008236. doi: 10.1371/journal.ppat.1008236. [DOI] [PMC free article] [PubMed] [Google Scholar]
231.Zhang L, Liu C, Li D, Zhao Y, Zhang X, Zeng X, et al. Antioxidant activity of an exopolysaccharide isolated from Lactobacillus plantarum C88. Int J Biol Macromol. 2013;54:270–5. doi: 10.1016/j.ijbiomac.2012.12.037. [DOI] [PubMed] [Google Scholar]
232.Li B, Du P, Smith EE, Wang S, Jiao Y, Guo L, et al. In vitro and in vivo evaluation of an exopolysaccharide produced by Lactobacillus helveticus KLDS1.8701 for the alleviative effect on oxidative stress. Food Funct. 2019;10:1707–17. doi: 10.1039/C8FO01920G. [DOI] [PubMed] [Google Scholar]
233.Zhou X, Zhang K, Qi W, Zhou Y, Hong T, Xiong T, et al. Exopolysaccharides from Lactobacillus plantarum NCU116 enhances colonic mucosal homeostasis by controlling epithelial cell differentiation and c-Jun/Muc2 signaling. J Agric Food Chem. 2019;67:9831–9. doi: 10.1021/acs.jafc.9b03939. [DOI] [PubMed] [Google Scholar]
234.Zhou X, Qi W, Hong T, Xiong T, Gong D, Xie M, et al. Exopolysaccharides from Lactobacillus plantarum NCU116 regulate intestinal barrier function via STAT3 signaling pathway. J Agric Food Chem. 2018;66:9719–27. doi: 10.1021/acs.jafc.8b03340. [DOI] [PubMed] [Google Scholar]
235.Sims IM, Ryan JLJ, Kim SH. In vitro fermentation of prebiotic oligosaccharides by Bifidobacterium lactis HN019 and Lactobacillus spp. Anaerobe. 2014;25:11–7. doi: 10.1016/j.anaerobe.2013.11.001. [DOI] [PubMed] [Google Scholar]
236.İspirli H, Demirbaş F, Dertli E. Glucan type exopolysaccharide (EPS) shows prebiotic effect and reduces syneresis in chocolate pudding. J Food Sci Technol. 2018;55:3821–6. doi: 10.1007/s13197-018-3181-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
237.Rios-Covian D, Cuesta I, Alvarez-Buylla JR, Ruas-Madiedo P, de Gueimonde M. Los Reyes-Gavilán CG. Bacteroides fragilis metabolises exopolysaccharides produced by bifidobacteria. BMC Microbiol. 2016;16:150. doi: 10.1186/s12866-016-0773-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
238.Rodrigues L, Banat IM, Teixeira J, Oliveira R. Biosurfactants: potential applications in medicine. J Antimicrob Chemother. 2006;57:609–18. doi: 10.1093/jac/dkl024. [DOI] [PubMed] [Google Scholar]
239.Franzetti A, Tamburini E, Banat IM. Applications of biological surface active compounds in remediation technologies. In: Sen R, editor. Biosurfactants. New York: Springer New York; 2010. pp. 121–34. [DOI] [PubMed] [Google Scholar]
240.Van Hamme JD, Singh A, Ward OP. Physiological aspects. Part 1 in a series of papers devoted to surfactants in microbiology and biotechnology. Biotechnol Adv. 2006;24:604–20. doi: 10.1016/j.biotechadv.2006.08.001. [DOI] [PubMed] [Google Scholar]
241.Naughton PJ, Marchant R, Naughton V, Banat IM. Microbial biosurfactants: current trends and applications in agricultural and biomedical industries. J Appl Microbiol. 2019;127:12–28. doi: 10.1111/jam.14243. [DOI] [PubMed] [Google Scholar]
242.Mujumdar S, Joshi P, Karve N. Production, characterization, and applications of bioemulsifiers (BE) and biosurfactants (BS) produced by Acinetobacter spp.: a review. J Basic Microbiol. 2019;59:277–87. doi: 10.1002/jobm.201800364. [DOI] [PubMed] [Google Scholar]
243.Mouafo TH, Mbawala A, Ndjouenkeu R. Effect of different carbon sources on biosurfactants’ production by three strains of Lactobacillus spp. Biomed Res Int. 2018;2018:1–15. doi: 10.1155/2018/5034783. [DOI] [PMC free article] [PubMed] [Google Scholar]
244.Haque F, Alfatah M, Ganesan K, Bhattacharyya MS. Inhibitory effect of sophorolipid on Candida albicans biofilm formation and hyphal growth. Sci Rep. 2016;6:23575. doi: 10.1038/srep23575. [DOI] [PMC free article] [PubMed] [Google Scholar]
245.Itapary Dos Santos C, Ramos Franca Y, Duarte Lima Campos C, Quaresma Bomfim MR, Oliveira Melo B, Assuncao Holanda R, et al. Antifungal and antivirulence activity of vaginal Lactobacillus spp. products against Candida vaginal isolates. Pathogens. 2019;8:150. doi: 10.3390/pathogens8030150. [DOI] [PMC free article] [PubMed] [Google Scholar]
246.Ceresa C, Tessarolo F, Caola I, Nollo G, Cavallo M, Rinaldi M, et al. Inhibition of Candida albicans adhesion on medical-grade silicone by a Lactobacillus-derived biosurfactant. J Appl Microbiol. 2015;118:1116–25. doi: 10.1111/jam.12760. [DOI] [PubMed] [Google Scholar]
247.Morais IMC, Cordeiro AL, Teixeira GS, Domingues VS, Nardi RMD, Monteiro AS, et al. Biological and physicochemical properties of biosurfactants produced by Lactobacillus jensenii P6A and Lactobacillus gasseri P65. Microb Cell Fact. 2017;16:155. doi: 10.1186/s12934-017-0769-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
248.Gudiña EJ, Teixeira JA, Rodrigues LR. Isolation and functional characterization of a biosurfactant produced by Lactobacillus paracasei. Colloids Surf B Biointerfaces. 2010;76:298–304. doi: 10.1016/j.colsurfb.2009.11.008. [DOI] [PubMed] [Google Scholar]
249.Spurbeck RR, Arvidson CG. Lactobacillus gasseri surface-associated proteins inhibit Neisseria gonorrhoeae adherence to epithelial cells. Infect Immun. 2012;80:3743. doi: 10.1128/IAI.00789-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
250.Foschi C, Salvo M, Cevenini R, Parolin C, Vitali B, Marangoni A. Vaginal lactobacilli reduce Neisseria gonorrhoeae viability through multiple strategies: an in vitro study. Front Cell Infect Microbiol. 2017;7:502. doi: 10.3389/fcimb.2017.00502. [DOI] [PMC free article] [PubMed] [Google Scholar]
251.Jiang X, Yan X, Gu S, Yang Y, Zhao L, He X, et al. Biosurfactants of Lactobacillus helveticus for biodiversity inhibit the biofilm formation of Staphylococcus aureus and cell invasion. Future Microbiol. 2019;14::1133–46. doi: 10.2217/fmb-2018-0354. [DOI] [PubMed] [Google Scholar]
252.Satpute SK, Mone NS, Das P, Banat IM, Banpurkar AG. Inhibition of pathogenic bacterial biofilms on PDMS based implants by L. acidophilus derived biosurfactant. BMC Microbiol. 2019;19::39. doi: 10.1186/s12866-019-1412-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
253.De Gregorio PR, Parolin C, Abruzzo A, Luppi B, Protti M, Mercolini L, et al. Biosurfactant from vaginal Lactobacillus crispatus BC1 as a promising agent to interfere with Candida adhesion. Microb Cell Fact. 2020;19:133. doi: 10.1186/s12934-020-01390-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
254.Oleksy-Sobczak M, Klewicka E. Optimization of media composition to maximize the yield of exopolysaccharides production by Lactobacillus rhamnosus strains. Probiotics Antimicrob Proteins. 2020;12:774–83. doi: 10.1007/s12602-019-09581-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
255.Fraunhofer ME, Jakob F, Vogel RF. Influence of different sugars and initial pH on β-glucan formation by Lactobacillus brevis TMW 1.2112. Curr Microbiol. 2018;75:794–802. doi: 10.1007/s00284-018-1450-z. [DOI] [PubMed] [Google Scholar]
256.Banat IM, Satpute SK, Cameotra SS, Patil R, Nyayanit NV. Cost effective technologies and renewable substrates for biosurfactants’ production. Front Microbiol. 2014;5:697. doi: 10.3389/fmicb.2014.00697. [DOI] [PMC free article] [PubMed] [Google Scholar]
257.Bertrand B, Martínez-Morales F, Rosas-Galván NS, Morales-Guzmán D, Trejo-Hernández MR. Statistical design, a powerful tool for optimizing biosurfactant production: a review. Colloids Interfaces. 2018;2:36. doi: 10.3390/colloids2030036. [DOI] [Google Scholar]
258.Li N, Wang Y, Zhu P, Liu Z, Guo B, Ren J. Improvement of exopolysaccharide production in Lactobacillus casei LC2W by overexpression of NADH oxidase gene. Microbiol Res. 2015;171:73–7. doi: 10.1016/j.micres.2014.12.006. [DOI] [PubMed] [Google Scholar]
259.Reid G. The need to focus on therapy instead of associations. Front Cell Infect Microbiol. 2019;9:327. doi: 10.3389/fcimb.2019.00327. [DOI] [PMC free article] [PubMed] [Google Scholar]
260.Ravel J, Brotman RM. Translating the vaginal microbiome: gaps and challenges. Genome Med. 2016;8:35. doi: 10.1186/s13073-016-0291-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
261.Ling Z, Liu X, Chen W, Luo Y, Yuan L, Xia Y, et al. The restoration of the vaginal microbiota after treatment for bacterial vaginosis with metronidazole or probiotics. Microb Ecol. 2013;65:773–80. doi: 10.1007/s00248-012-0154-3. [DOI] [PubMed] [Google Scholar]
262.Petrova MI, Lievens E, Malik S, Imholz N, Lebeer S. Lactobacillus species as biomarkers and agents that can promote various aspects of vaginal health. Front Physiol. 2015;6:81. doi: 10.3389/fphys.2015.00081. [DOI] [PMC free article] [PubMed] [Google Scholar]
263.Romero R, Hassan SS, Gajer P, Tarca AL, Fadrosh DW, Nikita L, et al. The composition and stability of the vaginal microbiota of normal pregnant women is different from that of non-pregnant women. Microbiome. 2014;2:4. doi: 10.1186/2049-2618-2-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
264.Vitali B, Pugliese C, Biagi E, Candela M, Turroni S, Bellen G, et al. Dynamics of vaginal bacterial communities in women developing bacterial vaginosis, candidiasis, or no infection, analyzed by PCR-denaturing gradient gel electrophoresis and real-time PCR. Appl Environ Microbiol. 2007;73:5731–41. doi: 10.1128/AEM.01251-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
265.Zhou X, Westman R, Hickey R, Hansmann MA, Kennedy C, Osborn TW, et al. Vaginal microbiota of women with frequent vulvovaginal candidiasis. Infect Immun. 2009;77:4130–5. doi: 10.1128/IAI.00436-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
266.Liu M-B, Xu S-R, He Y, Deng G-H, Sheng H-F, Huang X-M, et al. Diverse vaginal microbiomes in reproductive-age women with vulvovaginal candidiasis. PLoS One. 2013;8:e79812. doi: 10.1371/journal.pone.0079812. [DOI] [PMC free article] [PubMed] [Google Scholar]
267.Mayer BT, Srinivasan S, Fiedler TL, Marrazzo JM, Fredricks DN, Schiffer JT. Rapid and profound shifts in the vaginal microbiota following antibiotic treatment for bacterial vaginosis. J Infect Dis. 2015;212:793–802. doi: 10.1093/infdis/jiv079. [DOI] [PMC free article] [PubMed] [Google Scholar]
268.Freitas AC, Chaban B, Bocking A, Rocco M, Yang S, Hill JE, et al. The vaginal microbiome of pregnant women is less rich and diverse, with lower prevalence of Mollicutes, compared to non-pregnant women. Sci Rep. 2017;7:9212. doi: 10.1038/s41598-017-07790-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
269.Jespers V, Kyongo J, Joseph S, Hardy L, Cools P, Crucitti T, et al. A longitudinal analysis of the vaginal microbiota and vaginal immune mediators in women from sub-Saharan Africa. Sci Rep. 2017;7:11974. doi: 10.1038/s41598-017-12198-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
270.Nowak RG, Randis TM, Desai P, He X, Robinson CK, Rath JM, et al. Higher levels of a cytotoxic protein, vaginolysin, in Lactobacillus-deficient community state types at the vaginal mucosa. Sex Transm Dis. 2018;45:e14-7. doi: 10.1097/OLQ.0000000000000774. [DOI] [PMC free article] [PubMed] [Google Scholar]
271.Ata B, Yildiz S, Turkgeldi E, Brocal VP, Dinleyici EC, Moya A, et al. The endobiota study: comparison of vaginal, cervical and gut microbiota between women with stage 3/4 endometriosis and healthy controls. Sci Rep. 2019;9:2204. doi: 10.1038/s41598-019-39700-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
272.Borgogna JC, Shardell MD, Santori EK, Nelson TM, Rath JM, Glover ED, et al. The vaginal metabolome and microbiota of cervical HPV-positive and HPV-negative women: a cross-sectional analysis. BJOG. 2020;127:182–92. doi: 10.1111/1471-0528.15981. [DOI] [PMC free article] [PubMed] [Google Scholar]
273.Tortelli BA, Lewis WG, Allsworth JE, Member-Meneh N, Foster LR, Reno HE, et al. Associations between the vaginal microbiome and Candida colonization in women of reproductive age. Am J Obstet Gynecol. 2020;222:471.e1–471.e9. doi: 10.1016/j.ajog.2019.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
274.Verwijs MC, Agaba SK, Darby AC, van de Wijgert JHHM. Impact of oral metronidazole treatment on the vaginal microbiota and correlates of treatment failure. Am J Obstet Gynecol. 2020;222:157.e1–157.e13. doi: 10.1016/j.ajog.2019.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]

發表留言